Partial Knee Replacement Surgery
A targeted approach for localised knee arthritis
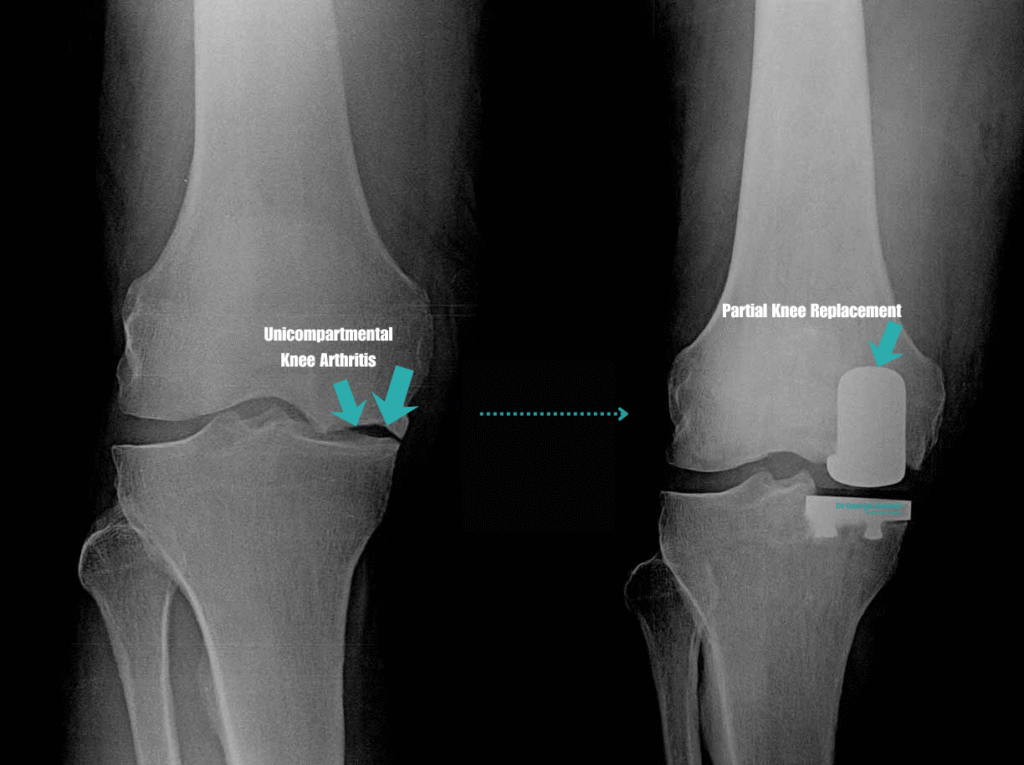
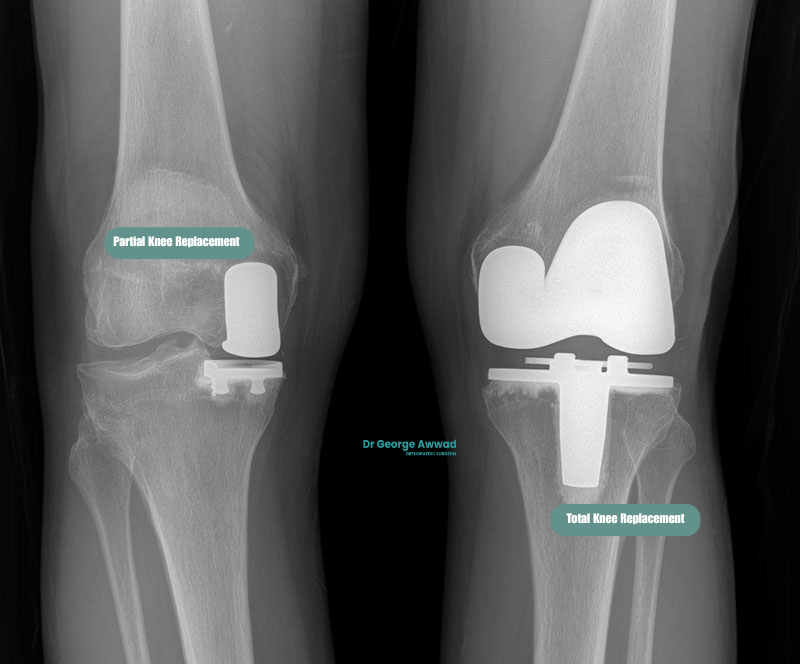
Partial knee replacement surgery, also known as unicompartmental knee arthroplasty, is a surgical procedure used to treat arthritis that affects only one part of the knee joint. Unlike total knee replacement, which replaces the entire joint surface, a partial knee replacement involves resurfacing only the damaged compartment, typically the medial (inner), lateral (outer), or patellofemoral (kneecap) region, while preserving healthy bone, cartilage, and ligaments.
This procedure may be considered if your arthritis is limited to a single area of the knee and non-surgical treatments such as physiotherapy, activity modification, or joint injections are no longer providing sufficient relief.
What is a partial knee replacement?
A partial knee replacement, also known as unicompartmental or, hemi knee arthroplasty, is a surgical procedure used to treat arthritis or damage that is limited to a single compartment of the knee joint. Unlike a total knee replacement, which replaces all the surfaces of the knee, a partial knee replacement targets only the affected area, either the medial (inner), lateral (outer), or patellofemoral (kneecap) compartment.
The goal of this surgery is to relieve pain, restore mobility, and maintain as much of the knee’s natural structure and movement as possible. Because the healthy parts of the knee are left intact, many patients find that their knee feels more natural after recovery compared to a total knee replacement. The cruciate ligaments (particularly the ACL) are typically preserved, which may help retain more natural knee kinematics.
Understanding the Terminology: Unicompartmental vs Partial vs Hemi Knee Replacement
These three terms; unicompartmental, partial, and hemi knee replacement, are often used interchangeably in clinical settings, and all refer to the same general surgical approach: replacing only the damaged portion of the knee joint, rather than the entire joint. Here’s how each term relates:
- Partial Knee Replacement - This is the most commonly used term in Australia and refers to any knee replacement procedure where only one part (compartment) of the knee joint is resurfaced. A partial knee replacement involves replacing only the compartment that is affected by arthritis or damage, leaving the healthy bone, cartilage, and ligaments untouched. It is often performed using a minimally invasive approach and may result in a faster recovery, more natural knee movement, and preservation of normal joint function.
- Unicompartmental Knee Replacement - This term is often used synonymously with partial knee replacement. It specifically refers to replacing just one of the tibiofemoral compartments, usually the medial or lateral. So a medial unicompartmental knee replacement is the most common form of partial knee surgery, used when osteoarthritis is isolated to the inner side of the knee.
- Hemi Knee Replacement - The term hemi means "half," and hemi knee replacement is another way to describe a unicompartmental or partial knee replacement, most commonly when one tibiofemoral compartment is involved. This term is less frequently used in Australian practice but may be encountered in international literature or surgical discussions.
When is partial knee replacement surgery recommended?
- You have osteoarthritis limited to a single compartment
- Non-surgical treatments such as physiotherapy or injections are no longer effective
- The ligaments in your knee (such as the ACL) remain intact and functioning
- You still have a good range of motion in the knee
- Imaging confirms that other parts of the joint are relatively well preserved
How is partial knee arthritis different from total knee arthritis?
Knee arthritis does not always affect the entire joint. In many patients, the wear and tear is isolated to a specific region, or “compartment,” of the knee. Understanding the difference between partial and total knee arthritis can help clarify whether a partial knee replacement may be a suitable surgical option.
Partial knee arthritis (unicompartmental disease)
Partial knee arthritis occurs when the degenerative changes are limited to just one of the three main compartments of the knee:
- Medial compartment (inner side of the knee)
- Lateral compartment (outer side)
- Patellofemoral compartment (behind the kneecap)
In these cases, the other compartments of the knee remain healthy, and the supporting ligaments such as the ACL and PCL are still functioning. Patients with partial knee arthritis often experience pain, stiffness, or swelling that is localised to one side of the knee or behind the kneecap, rather than throughout the entire joint.
Total knee arthritis (tricompartmental disease)
Total knee arthritis, or tricompartmental osteoarthritis, involves degenerative changes across all three compartments of the knee. This more widespread damage often results in:
- Diffuse pain throughout the entire knee
- Significant stiffness and loss of motion
- Deformity (such as bowing or knock-knee)
- Advanced cartilage loss
- Instability or difficulty walking even short distances
Patients with this level of joint degeneration are more likely to require a total knee replacement, which involves resurfacing the entire joint with prosthetic components.
Why this distinction matters
The type and distribution of arthritis in your knee is a major factor in determining which treatment is most appropriate. If arthritis is isolated and the rest of the knee is well-preserved, partial knee replacement may be considered. This allows preservation of natural structures and may offer a quicker recovery and more natural knee feel after surgery.
Your eligibility for either approach will be based on imaging, clinical examination, and a detailed understanding of your symptoms and activity goals.
Am I a candidate for partial knee replacement surgery?
Partial knee replacement surgery is not suitable for everyone with knee arthritis. It is typically considered when the damage is confined to a single compartment of the knee, and the rest of the joint remains healthy and well-aligned. Whether you are a good candidate will depend on your clinical symptoms, imaging results, and overall knee function.
Key factors that may indicate suitability
- Your arthritis is limited to only one compartment of the knee (medial, lateral or patellofemoral)
- You have moderate to severe pain that affects your daily activities despite trying non-surgical treatments
- Your knee retains a good range of motion, and your ligaments (ACL/PCL) are intact
- You do not have significant knee instability or deformity
- You are not significantly overweight, which can increase wear and risk of complications
- You are in generally good health and able to participate in a structured recovery and rehabilitation program
Imaging and clinical assessment
Individualised assessment
Dr Awwad will conduct a thorough clinical evaluation to determine whether a partial or total knee replacement is more appropriate for your specific condition. The goal is to recommend the surgical approach that offers the best potential outcome, while preserving as much of your natural joint as possible when suitable.
Who may not be suitable for partial knee replacement?
Situations where partial knee replacement may not be appropriate
- More than one compartment is affected: If arthritis involves multiple areas of the knee (medial, lateral, and/or patellofemoral), a total knee replacement may offer more comprehensive symptom relief.
- Significant ligament damage: Partial knee replacement relies on intact ligaments (especially the anterior cruciate ligament) to support knee stability and joint mechanics. If your ACL or PCL is torn or unstable, total replacement may be more appropriate.
- Severe deformity or joint misalignment: Marked bowing (varus) or knock-knee (valgus) deformity can limit the effectiveness of a partial knee replacement and increase the risk of early failure.
- Inflammatory or systemic joint disease: Conditions such as rheumatoid arthritis or other autoimmune diseases typically affect the entire joint, making a total knee replacement more suitable.
- Advanced stiffness or reduced range of motion: If your knee joint has become very stiff or lacks flexibility, you may not benefit fully from a partial replacement.
- High physical demands or obesity: In patients with a very high body mass index or those engaging in strenuous activity, the increased stress on the remaining compartments may reduce the lifespan of a partial implant.
- Previous major knee surgery: Certain prior procedures can alter the joint structure or mechanics, reducing the suitability for a partial knee implant.
Careful clinical assessment is essential
What are the benefits of partial knee replacement compared to total knee replacement?
Smaller incision and less disruption to soft tissue
Faster recovery and shorter hospital stay
Partial knee replacement may involve a shorter hospital stay and a faster return to walking and daily activities. Many patients experience less post-operative pain and swelling compared to total knee replacement, which may help them progress more quickly through early rehabilitation.
More natural knee motion
Preserving the unaffected parts of your knee may allow for more natural joint mechanics. Some patients report that their knee “feels more normal” after partial replacement compared to a total knee prosthesis, particularly with activities that require balance or coordination.
Reduced blood loss and lower risk of complications
Potential for future total knee replacement if needed

What are the limitations of partial knee replacement?
While partial knee replacement offers several benefits, it is not suitable for all patients or all patterns of knee arthritis. Understanding the limitations of the procedure is an important part of determining whether it is the most appropriate surgical option for you.
Only one compartment of the knee is treated
Partial knee replacement addresses arthritis in a single compartment of the knee, typically the medial (inner), lateral (outer), or patellofemoral (kneecap) region. If arthritis exists in more than one area or progresses to other compartments after surgery, further treatment may be required. In these cases, total knee replacement may offer more comprehensive long-term relief.
May not be suitable for patients with inflammatory arthritis
Patients with inflammatory conditions such as rheumatoid arthritis may experience widespread joint inflammation, affecting multiple compartments of the knee. In these cases, total knee replacement is often considered more appropriate.
Risk of needing further surgery
While many patients experience long-term symptom relief from a partial knee replacement, some may require revision surgery in the future, either to replace the worn implant or to convert to a total knee replacement if arthritis progresses. The long-term durability of partial implants may be less predictable than total knee replacements, especially in highly active patients.
Precision in patient selection and technique is critical
Partial knee replacement demands precise patient selection, imaging assessment, and surgical technique. Even small inaccuracies in implant positioning or soft tissue balance may affect joint function or lead to early wear. Surgeons with experience in partial knee replacement and access to advanced technologies such as robotic assistance may help reduce this risk.
Less common than total knee replacement
Because fewer patients meet the criteria for partial knee replacement, the procedure is performed less frequently than total knee replacement. As a result, not all orthopaedic surgeons offer this procedure, and some may prefer total knee replacement due to its broader applicability and established outcomes.
What surgical techniques are used in partial knee replacement?
Minimally invasive surgical approach
Partial knee replacement is typically performed using a minimally invasive approach through a smaller incision compared to total knee replacement. This technique involves carefully separating the muscles and tissues without cutting through major structures, which may help reduce post-operative pain and accelerate early mobility.
Robotic-assisted partial knee replacement
Personalised pre-operative planning
Bone resurfacing and implant placement
How does robotic-assisted technology support precision in partial knee replacement?
Enhanced pre-operative planning with 3D modelling
Real-time feedback during surgery
Improved implant positioning and alignment
- Reduced post-operative pain
- Better preservation of healthy bone and tissue
- More natural joint movement
- Lower rates of implant loosening or revision
Surgeon-controlled technology
What is involved in a personalised surgical plan for partial knee replacement?
Detailed assessment and imaging
- The extent and location of arthritis (usually confined to the medial, lateral, or patellofemoral compartment)
- The shape and orientation of your bones
- The alignment of your leg (e.g. bow-legged or knock-kneed)
- The integrity of surrounding ligaments and cartilage
3D modelling and surgical simulation
- Precise bone cuts to remove only the damaged area
- Implant placement that restores natural joint alignment
- Preservation of healthy structures, such as ligaments and cartilage
Alignment goals and soft tissue balance
Unlike a “one-size-fits-all” approach, a personalised plan takes into account your natural knee kinematics; how your knee moves and bears load. Dr Awwad may use kinematic alignment principles, which aim to reproduce your original joint movement and function, rather than artificially straightening the limb at all costs. Balancing the soft tissues around the knee is also a key part of the plan. This helps ensure the joint feels stable and moves comfortably after surgery.
Robotic-assisted execution
If robotic-assisted technology is used during surgery, the personalised plan is loaded into the system to guide the procedure. This allows Dr Awwad to execute the plan with sub-millimetre precision, adjusting in real time if needed based on how your knee behaves during surgery.
- A predefined map of where to remove damaged bone
- Boundaries to protect surrounding tissue
- Feedback on joint tension and movement
This combination of pre-operative planning and intra-operative technology supports consistent, high-quality outcomes.
Why personalisation matters
- Reduce pain
- Improve joint stability
- Enhance recovery
- Maximise implant longevity
- Support a more natural-feeling joint
What type of implant is used in partial knee replacement?
Partial knee replacement surgery involves resurfacing only the damaged portion of the knee joint, typically the medial (inner), lateral (outer) or patellofemoral (front) compartment. The healthy cartilage, bone, and ligaments in the unaffected parts of the knee are preserved. The prosthetic components are designed to restore smooth, stable movement while maintaining as much of the knee’s natural function as possible.
Implant components and design
A typical partial knee implant has three key parts:
- Femoral component: A contoured metal piece that resurfaces the end of the femur (thigh bone).
- Tibial component: A flat metal tray that resurfaces the top of the tibia (shinbone).
- Polyethylene bearing: A medical grade plastic spacer that sits between the femoral and tibial components, allowing for smooth, low friction gliding, similar to how healthy joint cartilage functions.
Because the anterior cruciate ligament (ACL) is usually preserved in partial knee replacement, many patients may experience a more natural-feeling knee compared with total knee replacement.

Cemented vs cementless fixation
In most cases, both the tibial and femoral components are cemented into place using a special surgical-grade bone cement, which provides immediate fixation and stability. Some modern implants are designed to be cementless, allowing bone to grow directly into the implant surface.
- Cemented fixation: is the most common technique. Bone cement provides immediate stability and is well supported by long-term registry data.
- Cementless fixation: is available in some modern designs. These implants have porous surfaces that allow bone to grow into them over time. Cementless fixation may be considered in younger patients with strong bone quality.
The decision for which fixation is used is often dependent upon patient age and quality of the bone and both methods are accepted and supported by contemporary registry outcomes.
Fixed vs mobile bearing implants
- Fixed bearing: The plastic insert is securely attached to the tibial tray, offering predictable movement and stability. This is the most commonly used design and is suitable for most patients.
- Mobile bearing: The polyethylene insert is allowed a small amount of movement, which may mimic natural knee motion more closely and reduce long-term wear. However, mobile-bearing designs may be more technically demanding and are not always necessary for optimal outcomes.
Why implant design matters
Not all partial knee implants perform equally well. Differences in design, materials, fixation method, and how well the implant accommodates individual anatomy can affect long-term outcomes and the likelihood of revision surgery. To ensure the highest standards of care, all joint implants used in Australia are tracked through the Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR). This registry monitors long-term performance data, revision rates, and patient outcomes across a wide range of implant brands and models.
Dr Awwad’s implant selection
- Fit a wide range of anatomies
- Allow for precise alignment and soft tissue balance
- Provide reliable, reproducible outcomes
- Minimise the risk of complications and revision
What does the recovery process look like after partial knee replacement?
Immediately after surgery
- Hospital stay: Most patients stay in hospital for 1–2 days.
- Pain management: Medications are provided to help manage pain and reduce inflammation during the early postoperative period.
- Mobilisation: You will be encouraged to start moving your leg and walking (with assistance) within hours of surgery. Early mobilisation helps reduce the risk of blood clots and promotes faster recovery.
First 2 weeks after surgery
- Wound care: You’ll be given instructions for keeping the surgical wound clean and dry. Dressings are usually removed after 14 days.
- Walking aids: Most people use crutches or a walking frame for support during the first week or two. As strength and balance improve, you may progress to walking unaided.
- Swelling and stiffness: It is normal to experience some swelling, tightness, and reduced range of motion early in the recovery. Icing and elevation can help reduce discomfort.
Physiotherapy and rehabilitation
- Exercise program: Physiotherapy usually begins immediately after surgery, either while you are in hospital or shortly after discharge. Your physiotherapist will guide you through a personalised program focused on:
- Regaining range of motion
- Improving strength in the thigh and calf muscles
- Enhancing balance and walking patterns
- Home or outpatient rehab: Some patients continue rehab at home, while others attend outpatient physiotherapy clinics. The intensity and frequency of sessions will be adjusted based on your needs and goals.
6–12 weeks after surgery
- Improved function: Most patients return to regular daily activities such as walking, climbing stairs, and light household tasks within 6 weeks.
- Driving: Many patients feel confident to drive again around the 4–6-week mark, particularly once they can fully bend the knee and safely operate pedals. Always check with your surgeon for clearance.
- Return to work: Depending on your occupation, you may be able to return to work within 3–6 weeks (for desk-based roles) or a little longer if your job involves more physical demands.
Long-term recovery
- Activity levels: After 3 months, many patients resume recreational activities such as swimming, cycling, or golf. High-impact sports are usually discouraged to protect the longevity of the implant.
- Follow-up: Dr Awwad will monitor your recovery with follow-up appointments and periodic imaging to ensure the implant is functioning well.
Key recovery benefits with partial knee replacement
- Less postoperative pain and swelling
- Quicker return of mobility
- Shorter hospital stay
- Faster rehabilitation milestones
- A more “natural” feeling knee due to preservation of native ligaments and joint surfaces
When can I return to walking, driving, and work after partial knee replacement?
Walking
- Week 1–2: Walking short distances indoors with crutches or a frame. Some patients can begin weaning off walking aids within the first two weeks.
- Week 2–4: Increased walking capacity around the home and outdoors. Many patients can walk unaided on flat surfaces.
- Week 4–6: Most people are walking independently, with confidence on stairs and uneven ground gradually improving.
Driving
- Most patients are able to return to driving between 4–6 weeks after surgery, once they can:
- Bend the knee comfortably to operate pedals
- Perform an emergency stop safely
- Are no longer taking strong opioid pain medication
Returning to work
- Sedentary jobs (e.g. office work): Many patients return between 3–6 weeks post-surgery if they can sit comfortably, manage stairs, and commute safely.
- Standing or light manual jobs: These may require 6–8 weeks of recovery before returning.
- Physically demanding jobs (e.g. construction, trades, healthcare): You may need 8–12 weeks or more off, especially if kneeling, lifting, or climbing is required.
Summary
| Activity | Typical Return Time |
|---|---|
| Walking with support | Same day to 1 day post- |
| Walking independent | 2–6 weeks |
| Driving | 4–6 weeks (with clearance |
| Return to desk work | 3–6 weeks |
| Return to physical work | 6–12 weeks |
Is physiotherapy required after partial knee replacement surgery?
Why physiotherapy matters after partial knee replacement
- Improving knee movement and range of motion
- Strengthening muscles around the knee and hip
- Re-training your walking pattern (gait) to avoid limping or compensatory habits
- Preventing stiffness and scar tissue formation
- Reducing swelling and pain with targeted strategies
- Supporting balance and coordination
- Helping you safely return to daily activities, work, and exercise
When physiotherapy begins
- Immediately after surgery: While still in hospital, you’ll usually begin gentle exercises and start walking with the help of physiotherapy staff.
- Early recovery (first 2–6 weeks): Your physiotherapist will provide exercises to improve knee mobility and start strengthening.
- Later phases (6 weeks and beyond): The focus shifts to more advanced strengthening, balance training, and return to specific functional or occupational tasks.
Personalised exercise plan
- The compartment of the knee replaced (medial, lateral, or patellofemoral)
- Your overall health and fitness
- Your lifestyle goals and activity level
- Your progress during early recovery
How long will I need physiotherapy?
Most patients benefit from at least 6–12 weeks of guided physiotherapy, although some may continue longer depending on their needs and goals. Ongoing home exercises are usually recommended for several months to maintain strength and function.
In summary, physiotherapy is essential for achieving the best possible outcome from your partial knee replacement. It supports faster recovery, safer return to activities, and better long-term function of your new joint. Your physiotherapy plan will be carefully aligned with your surgery and your personal recovery goals.
What are the potential risks or complications?
- Infection: As with any surgery, there is a risk of infection at the surgical site or within the joint. Preventative measures such as antibiotics and sterile techniques are used to minimise this risk.
- Blood clots: Deep vein thrombosis (DVT) or pulmonary embolism can occur after joint surgery. Blood-thinning medication, early mobilisation, and compression devices are often used to help prevent this.
- Implant-related complications: These can include loosening, wear, or breakage of the prosthetic components over time. If this occurs, revision surgery may be needed.
- Stiffness or reduced range of motion: While many patients regain good movement, scar tissue or joint stiffness can occasionally limit range of motion.
- Nerve or blood vessel injury: Although rare, there is a small risk of injury to nearby nerves or blood vessels during surgery.
- Persistent pain: Some patients may experience ongoing discomfort after surgery, even when the implant is functioning well. This can be due to soft tissue irritation, mechanical issues, or other causes unrelated to the implant.
- Change in knee alignment or function: In some cases, the alignment or balance of the knee may feel different after surgery. Robotic-assisted techniques and personalised surgical planning aim to reduce this risk by improving implant positioning and joint balance.
- Reoperation or revision surgery: Though partial knee replacement aims to preserve as much of the healthy knee as possible, the remaining compartments may develop arthritis over time. This may eventually require conversion to a total knee replacement if symptoms become severe.
Minimising risk through careful planning and modern techniques
Dr Awwad utilises modern surgical planning tools, established surgical techniques, and where appropriate, robotic-assisted technology to support accuracy during knee replacement procedures. These approaches aim to enhance implant positioning and joint function. Post-operative care, including physiotherapy and clinical monitoring, is an important part of the recovery process and may assist in reducing the likelihood of complications.
If you have medical conditions or risk factors such as smoking, diabetes, or obesity, these will be reviewed and taken into account as part of your surgical planning and post-operative care. Dr Awwad will discuss strategies that may help optimise your health and recovery outcomes.
Partial knee replacement vs total knee replacement: which is right for you?
If you’re living with knee arthritis, one of the most important decisions in your treatment journey is whether to have a partial knee replacement (PKR) or a total knee replacement (TKR). Both procedures aim to relieve pain and improve function, but they differ in terms of surgical approach, recovery, and long-term considerations. The most appropriate option for you depends on the extent of arthritis in your knee, your overall health, lifestyle, and goals.
Key differences between partial and total knee replacement
| Feature | Partial Knee Replacement (PKR) | Total Knee Replacement (TKR) |
|---|---|---|
| Extent of arthritis treated | One compartment only (typically medial, lateral, or patellofemoral) | Two or more compartments (always medial and lateral; patellofemoral joint may or may not be resurfaced) |
| Tissue preservation | Preserves more bone and ligaments | Replaces all joint surfaces and sometimes removes ligaments |
| Surgical invasiveness | Smaller incision, less bone removal | Larger incision, more comprehensive reconstruction |
| Recovery time | Generally faster recovery and shorter hospital stay | Longer initial recovery, more extensive physiotherapy |
| Knee function | Often retains more natural movement and feel | Reliable pain relief, but may feel more artificial |
| Suitability | Best for patients with isolated compartment arthritis | Suitable for widespread arthritis across the entire knee |
| Revision risk | May require conversion to TKR in future if arthritis spreads | Typically lasts longer with fewer additional surgeries required |
Factors that influence the decision
1. Location and extent of arthritis
2. Knee stability and alignment
3. Age and activity level
4. Your health and surgical risk
A personalised approach with Dr George Awwad
Dr Awwad carefully evaluates each patient using physical examination, imaging studies, and detailed pre-operative planning tools to determine the best surgical option for your individual needs. His focus is on preserving as much of your natural knee function as possible while delivering lasting pain relief and joint stability. Whether you are suited to a partial or total knee replacement, Dr Awwad will provide you with the information, support, and surgical expertise to help you make the decision that best aligns with your health, lifestyle, and long-term goals.
Your partial knee replacement surgical journey with Dr George Awwad
Initial consultation and assessment
Pre-operative planning
- A review of your general health and any medical conditions
- Medication review and blood tests
- Prehabilitation exercises (if recommended)
- Information about your hospital admission, fasting, and discharge plan
Day of surgery
Surgical Procedure: Step-by-Step
1. Anaesthesia
- Spinal anaesthesia (most common), often combined with sedation, or
- General anaesthesia, based on your health status and anaesthetic preference.
2. Incision and Exposure
3. Bone Preparation
4. Implant Placement
5. Range of Motion Check
6. Wound Closure
7. After the procedure:
- You’ll be monitored in recovery and transferred to your hospital room
- Physiotherapy typically begins within hours of surgery
- Most patients walk with a frame or crutches the same day
Hospital stay and immediate post-operative care
- Your pain will be carefully managed
- A physiotherapist will assist you to begin walking, usually within 24 hours
- You will be given a mobility aid (such as crutches or a frame)
- Dr Awwad will review your progress and discuss the next steps
Recovery and rehabilitation
- Wound care instructions
- Medication guidance
- An individualised physiotherapy program to help regain strength, mobility, and confidence
- A timeline for returning to driving, work, and other daily activities
Follow-up with Dr Awwad
Post operatively you will return for a follow-up appointment with Dr Awwad. This consultation provides an opportunity to assess your wound healing, monitor your knee’s range of motion, and evaluate how your implant is functioning during daily activities.
Dr Awwad will also discuss your progress in physiotherapy and provide personalised guidance on safely increasing your activity levels. If you have any concerns during your recovery, Dr Awwad remains available to support you and adjust your care plan as needed.
Partial knee replacement surgery FAQs
How long will my partial knee replacement last?
The longevity of a partial knee replacement varies from person to person and depends on several factors, including age, activity level, body weight, bone quality, and how well the joint is cared for after surgery. Current research suggests that many partial knee replacements can last 10 to 15 years or more, particularly when performed in well-selected patients using modern implants and precise surgical techniques. In some cases, partial knee replacements have lasted well beyond this timeframe. To support the best possible outcome, Dr George Awwad uses high-performing implants, patient-specific planning, and may incorporate robotic-assisted techniques for enhanced precision.
If a partial knee replacement eventually wears out or fails, it is usually possible to revise it to a total knee replacement. The goal is always to achieve a durable result the first time, helping you maintain mobility and reduce discomfort for many years to come.
Can I return to sports after a partial knee replacement?
Many patients return to low-impact activities such as walking, swimming, cycling, and golf following recovery. Partial knee replacement may offer better preservation of natural movement, which can support return to some higher levels of activity compared to total knee replacement. That said, high-impact or contact sports such as running, jumping, or football are generally discouraged to avoid excessive stress on the implant. Dr Awwad will provide personalised advice based on your fitness level, goals, and implant type.
Is robotic-assisted surgery used in every case?
Dr Awwad offers robotic-assisted surgery where appropriate, as it allows for greater surgical accuracy and reproducibility. Not all patients may require or benefit from robotic technology, and Dr Awwad will discuss the best surgical approach for your individual case during your consultation.
Can I drive after partial knee replacement?
Most patients can return to driving within 4 to 6 weeks, once they are no longer taking strong pain medication, have regained sufficient strength and control in the operated leg, and feel safe behind the wheel. Always check with Dr Awwad before resuming driving.
Is the recovery faster than total knee replacement?
Yes, for suitable candidates, recovery from partial knee replacement is generally faster than that of a total knee replacement. Many patients experience less pain, quicker return to walking, and shorter hospital stays, particularly when combined with a minimally invasive surgical technique and enhanced recovery pathway.
Will I need physiotherapy?
Yes. Physiotherapy plays a vital role in restoring strength, flexibility, and confidence after your procedure. Dr Awwad works closely with experienced physiotherapists who will guide your progress from early mobilisation in hospital through to return to normal activity.
Are there risks involved in partial knee replacement?
Like all surgery, there are potential risks, including infection, blood clots, implant wear or loosening, stiffness, or ongoing discomfort. With careful patient selection, personalised planning, and modern techniques, these risks may be reduced. You will receive detailed information about risks and how they apply to your situation during your consultation with Dr Awwad.
How do I know if I need a total knee replacement instead?
Dr Awwad will assess your imaging and clinical symptoms to determine which parts of your knee are affected by arthritis. If your condition involves more than one compartment of the knee or if there are signs of instability, a total knee replacement may be more appropriate. Where possible, preserving healthy parts of the knee with a partial replacement can offer excellent outcomes.
What happens if the other compartments develop arthritis?
A partial knee replacement addresses arthritis that is limited to one compartment of the knee, most commonly the medial (inner), lateral (outer), or patellofemoral (kneecap) compartment. The remaining parts of the knee, which are not replaced during this surgery, are preserved to retain as much of your natural knee structure, function, and sensation as possible.
In some patients, arthritis may later develop in the previously unaffected compartments of the knee. This can lead to:
- New or recurring knee pain
- Stiffness or swelling
- Reduced function or instability
The rate and likelihood of arthritis progression vary depending on your individual knee anatomy, activity level, body weight, and underlying joint health. Some patients enjoy decades of excellent function without needing further surgery, while others may eventually require additional treatment.
Can a partial knee replacement be revised to a total knee replacement?
Yes. If arthritis progresses significantly, a conversion to total knee replacement (TKA) may be considered. This is a well-established procedure where the remaining parts of the joint are replaced. The revision is typically more straightforward when the original partial knee implant is still well-positioned and hasn’t caused bone loss or other issues.
Monitoring and prevention
To reduce the likelihood of arthritis progressing in the other compartments:
- Regular follow-up with your surgeon is important to monitor the knee’s overall health.
- Maintaining a healthy weight helps reduce stress across all areas of the joint.
- Strengthening exercises and physiotherapy can support joint stability and mobility.
- Managing underlying inflammatory or degenerative conditions such as rheumatoid arthritis or gout is also important.
How much does partial knee replacement surgery cost in Australia?
The cost of partial knee replacement surgery in Australia varies depending on several factors, including your level of private health insurance, the hospital where the procedure is performed, and whether robotic-assisted technology is used.
Privately insured patients
If you hold private health insurance, part or all of your hospital and surgical fees may be covered. Your exact out-of-pocket costs however, will depend on:
- The level of cover included in your policy
- Any excess payable
- Gaps charged by the surgeon, anaesthetist, or hospital
For privately insured patients, Dr Awwad charges a gap that will be discussed at the time of your appointment. Other out-of-pocket expenses, such as your health fund excess and the anaesthetist’s fee, will vary according to your individual policy.
Robotic-assisted partial knee replacement
Robotic-assisted surgery may involve additional costs related to pre-operative imaging (such as a CT scan) or the use of advanced robotic technology during the procedure. In some hospitals, these expenses are already included in the standard surgical package. In others, they may be itemised and billed separately. While robotic-assisted systems are designed to support greater accuracy in implant placement and alignment, their use may attract a small additional fee. Medicare rebates apply for eligible components of the procedure, and your private health insurer may cover some or all of the associated costs depending on your policy.
Self-funding patients
If you are uninsured or self-funding your surgery, a quote for surgery can be provided. This can vary depending on hospital choice and individual requirements. Our team can provide a personalised estimate and outline available payment options.
How to avoid unexpected expenses
To ensure you have a clear understanding of fees before surgery, we recommend:
- Requesting an itemised quote from Dr Awwad’s rooms
- Confirming your private health insurance coverage for joint replacement item numbers
- Asking whether robotic-assisted surgery and CT imaging are included in your policy or will attract an additional gap
Personalised cost estimate
After your consultation, Dr Awwad’s team will provide a tailored quote that includes:
- Surgeon’s fee
- Anaesthetist costs
- Hospital fees
- Any additional costs for robotic-assisted technology or imaging
This ensures you have a transparent understanding of your likely expenses before committing to surgery.
Who is the best partial knee replacement surgeon in Adelaide?
There is no single “best” partial knee replacement surgeon in Adelaide. The most appropriate surgeon for you depends on your individual condition, goals, and preferences. When making a decision, it may help to consider whether your surgeon has:
- Subspecialty training in knee arthroplasty, including partial (unicompartmental) knee replacement
- Experience with robotic-assisted, minimally invasive, or personalised surgical techniques
- A track record of safe outcomes and patient-centred care
- Clear, transparent information about implants, recovery expectations, and candidacy criteria
- Experience across both public hospital trauma work and private elective practice
Dr George Awwad holds subspecialty training in knee and hip surgery, including partial and total knee replacement procedures. His practice emphasises:
- Patient-specific surgical planning supported by advanced imaging
- Use of robotic-assisted technology where appropriate for accuracy in implant placement
- Minimally invasive approaches designed to support enhanced recovery
- A personalised approach, ensuring that both surgical and non-surgical options are carefully discussed with each patient
Dr Awwad consults at several locations across Adelaide and operates at both public and private hospitals. His focus is on helping patients make well-informed decisions about their treatment, with clear guidance from the first consultation through to rehabilitation.
