Medial Patellofemoral Ligament Reconstruction

Medial Patellofemoral Ligament Reconstruction
A surgical procedure to help stabilise the kneecap following recurrent patella dislocations
The medial patellofemoral ligament (MPFL) is one of the key soft tissue stabilisers that helps keep the kneecap (patella) aligned as your knee bends and straightens. When this ligament becomes stretched or torn, often due to trauma or recurrent patellar dislocations, the kneecap can become unstable, leading to pain, a feeling of giving way, and further dislocations.
MPFL reconstruction is a procedure that aims to restore stability to the patella by reconstructing the damaged ligament, usually with a graft from the patient’s own tissue. This may help reduce the risk of future dislocations, relieve discomfort, and improve knee function, particularly in young or active individuals.
Throughout this page, you’ll find detailed information on when MPFL reconstruction may be recommended, how the procedure is performed, recovery expectations, and answers to common patient questions.
What is the medial patellofemoral ligament (MPFL)?
The medial patellofemoral ligament (MPFL) is a key stabilising structure in your knee. It connects the inner edge of the patella (kneecap) to the femur (thigh bone) and plays a vital role in keeping the patella in place, especially during the first 20–30 degrees of knee bending.
The MPFL acts as a restraint against lateral (outward) movement of the patella. When functioning properly, it prevents the kneecap from slipping out of place, particularly during twisting or pivoting movements. It is especially important in younger patients or athletes, where kneecap stability is essential for active motion.
The MPFL is frequently torn or stretched during a patellar dislocation, which typically happens when the kneecap is forced outwards, often during sports or a traumatic event. Once damaged, the ligament may not heal properly on its own, leading to a higher risk of future dislocations or ongoing knee instability.
When MPFL reconstruction might be recommended
Medial patellofemoral ligament (MPFL) reconstruction may be recommended when non-surgical treatments have not adequately restored kneecap stability, or if the MPFL has been torn in a way that will not heal properly on its own.
Common reasons for surgery
- Recurrent patellar dislocations: If you have had multiple episodes of the kneecap dislocating, it often indicates that the MPFL has not healed or is insufficiently supporting the patella.
- Significant MPFL damage on imaging: MRI or clinical examination reveals a complete tear or severe elongation of the MPFL, especially if combined with instability.
- Persistent knee instability: Even without full dislocation, if the kneecap feels unstable, loose, or painful during movement—particularly during twisting, squatting, or climbing stairs—MPFL reconstruction may help.
- Failure of non-operative management: Bracing, physiotherapy, and activity modification have not improved symptoms or function.
- First-time dislocation in selected cases: In some young, active patients with high-risk anatomy (e.g. patella alta, trochlear dysplasia), surgery may be considered after a first-time dislocation to reduce the risk of recurrence.
Additional considerations
- Trochlear dysplasia (a shallow groove in the thigh bone)
- Patella alta (a high-riding kneecap)
- Increased tibial tubercle–trochlear groove [TT-TG] distance
- Rotational limb alignment issues
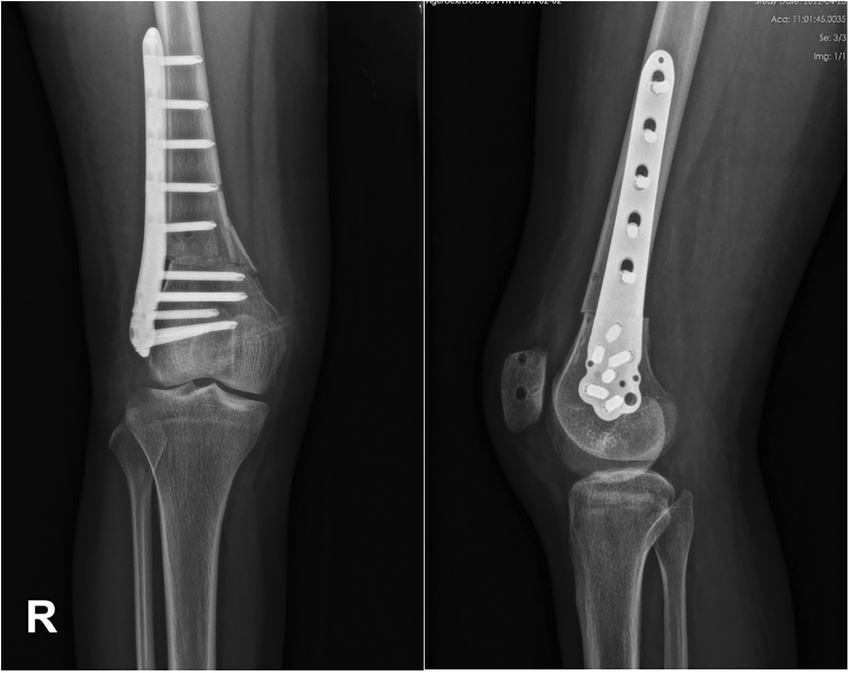
In some cases, MPFL reconstruction may be combined with other procedures, such as a tibial tubercle osteotomy (TTO), to better correct the alignment of the kneecap and reduce the risk of future dislocations.
How MPFL injuries are diagnosed
Diagnosing an injury to the medial patellofemoral ligament (MPFL) involves a combination of your medical history, a physical examination, and imaging tests. Accurate diagnosis helps determine the extent of damage and whether surgical reconstruction may be appropriate.
Clinical assessment
- Trochlear dysplasia (a shallow groove in the thigh bone)
- Patella alta (a high-riding kneecap)
- Increased tibial tubercle–trochlear groove [TT-TG] distance
- Rotational limb alignment issues
- Apprehension test: Gently pushing the kneecap laterally (to the outside) to assess whether you feel discomfort or a sense that it may dislocate.
- Patella glide and tilt tests: To assess how mobile the kneecap is and whether it is overly loose.
- Joint tracking: Observing how the kneecap moves during bending and straightening of the knee.
Imaging studies

X-rays
- Standard X-rays can show if the kneecap is abnormally positioned or if there is damage to the bone surfaces after a dislocation.
- Special views such as a skyline or Merchant view may be used to see how the patella sits in the groove of the femur.
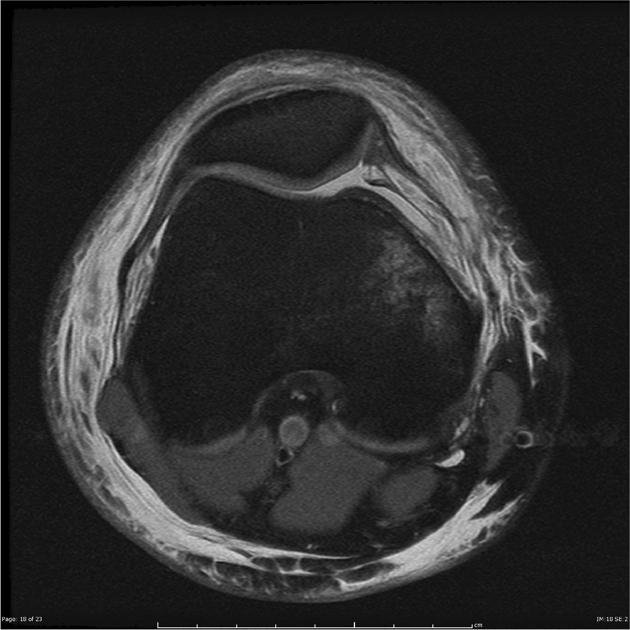
MRI (Magnetic Resonance Imaging)
- An MRI scan is the most useful test for visualising the MPFL and other soft tissues.
- It can show whether the MPFL is torn, stretched, or scarred, and whether there is associated cartilage or bone damage.
- MRI can also identify risk factors for ongoing instability, such as trochlear dysplasia or patella alta.
CT Scan (in select cases)
- Sometimes used for detailed measurements of bone alignment, such as the TT–TG (tibial tubercle to trochlear groove) distance.
- May help guide surgical planning if multiple structural issues are present.
Combined approach
Diagnosis is not based on a single test. Instead, it is the combination of history, clinical findings, and imaging results that leads to an accurate diagnosis and a tailored treatment plan. If MPFL reconstruction is being considered, Dr Awwad will ensure that contributing anatomical issues are also evaluated and, if needed, addressed during surgery.
Surgical technique for MPFL reconstruction
Graft choice and preparation
- Hamstring autograft (most commonly the gracilis tendon): harvested from the patient's own leg.
- Quadriceps tendon autograft: occasionally used in cases with specific anatomical considerations.
- Allograft (donor tissue): used in select cases, such as revision surgery or when autograft tissue is not suitable.
Surgical approach
- Arthroscopic or mini-open access: Small incisions are made to allow for visualisation of the joint and placement of the graft.
- Graft placement: The graft is anchored to both the femur (thigh bone) and the patella (kneecap) in a position that replicates the natural anatomy of the MPFL.
- Precise tensioning: Correct graft tension is essential to avoid over-tightening (which can cause stiffness or abnormal tracking) or under-tightening (which can result in continued instability).
- Fluoroscopic guidance: Intra-operative imaging may be used to assist in locating the optimal femoral attachment point and to confirm the patellar alignment throughout the knee’s range of motion.
Concurrent procedures
- Tibial Tubercle Osteotomy (TTO): to realign the patella.
- Lateral release: to release tight structures pulling the patella outwards.
- Cartilage repair techniques: if damage is present due to recurrent dislocations.
Fixation
Recovery and rehabilitation after MPFL surgery
Medial Patellofemoral Ligament (MPFL) reconstruction typically involves a structured recovery and rehabilitation plan aimed at protecting the reconstructed ligament, minimising pain and swelling, and gradually restoring strength and range of motion in the knee. Dr George Awwad’s post-operative protocol is designed to support safe healing and return to activity.
Immediately after surgery
- Hospital stay: Most patients return home the same day or after an overnight stay.
- Bracing: A knee brace is worn at all times (except during supervised therapy) for the first 4–6 weeks to protect the graft during early healing.
- Compression stockings: These are worn for 24–48 hours post-op to help reduce the risk of blood clots. You can discontinue their use once you are regularly walking.
Wound care and dressings
- Dressings: The bulky outer dressings can be removed the day after surgery, but adhesive dressings should remain intact. Protect the area when showering.
- Follow-up: A dressing change and wound check are scheduled 2 weeks post-operatively with a nurse.
Pain management and swelling control
- Pain relief: Pain medications such as Panadeine Forte, Tramadol, Palexia, or Endone may be prescribed. Anti-inflammatories are generally avoided unless specifically advised.
- Ice therapy: regular icing to control pain and swelling over the first 2 weeks. Ice can be continued beyond this if helpful.
- Elevation: Elevating the leg intermittently during the first 72 hours can also assist with swelling.
Rehabilitation milestones
Weeks 1–2
- Partial weight-bearing with crutches
- Knee brace locked in extension (worn full-time except during physio)
- Range of motion (ROM) exercises 0–90° (with supervision only)
Weeks 3–4
- Transition to full weight-bearing while still wearing brace
- Continue ROM exercises, progressing to 120°
Weeks 5–6
- Full weight-bearing in brace with ROM 0–90°
- Continue exercises as tolerated
Weeks 6–12
- Discontinue brace
- Begin full ROM exercises
- Focus on strengthening the leg
Week 12 onwards
- Jogging and sport-specific rehabilitation may begin, guided by physiotherapy and clinical review
- Driving: For left leg surgery in an automatic car, driving may resume after 1 week. For right leg surgery or manual cars, typically after 4 weeks.
- Work: Return to work will depend on your job and should be discussed with Dr Awwad.
When to seek medical attention
Contact Dr Awwad’s rooms or the hospital if you experience:
- High fever
- Worsening redness or swelling
- Excessive bleeding or discharge from the incision
- Calf pain or unusual leg swelling
Possible risks and complications of MPFL surgery
1. Infection
2. Blood clots (DVT)
3. Knee stiffness or reduced range of motion
4. Graft-related complications
- Graft stretching or failure
- Graft malpositioning, which could lead to abnormal patellar tracking
- Donor site pain or weakness if an autograft is used
5. Recurrent instability
6. Over-tightening of the graft
7. Pain at the kneecap (anterior knee pain)
8. Nerve or vascular injury
9. Hardware-related issues
10. Post-operative complications
Dr George Awwad will discuss these risks in detail during your consultation, considering your individual anatomy, activity level, and medical history. Your recovery will be closely monitored, and a structured rehabilitation plan will be implemented to help reduce complications and optimise your surgical outcome.
