Knee Osteotomy
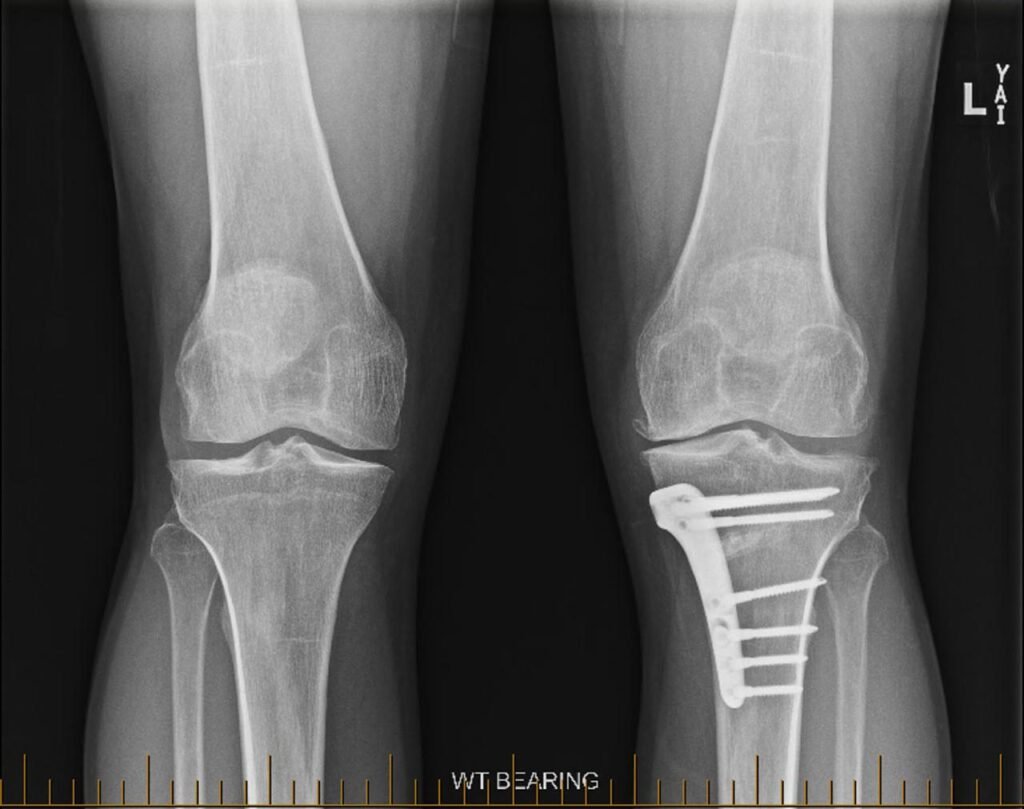
Realigning the knee joint to relieve pain and delay joint replacement
Knee osteotomy is a joint preservation procedure designed to shift the weight bearing load away from the damaged part of the knee joint. This surgery may be recommended for younger or more active patients with knee arthritis that is limited to one side of the knee. By adjusting the alignment of the leg, knee osteotomy can help reduce pain, improve function, and potentially delay the need for a total knee replacement.
Dr George Awwad offers knee osteotomy as part of his comprehensive approach to knee care, helping selected patients manage their arthritis while maintaining an active lifestyle.
What is a knee osteotomy?
A knee osteotomy is a surgical procedure that involves reshaping or repositioning one of the bones in the leg, either the tibia (shinbone) or femur (thighbone), to improve the alignment of the knee joint. This realignment helps shift weight away from a damaged or arthritic area of the knee, which may reduce pain and improve function in people with localised knee arthritis or deformity. Rather than replacing the knee joint with an implant, a knee osteotomy aims to preserve the patient’s natural joint for as long as possible. By redistributing pressure across the joint, the procedure can help slow the progression of arthritis and potentially delay or avoid the need for total knee replacement surgery.
Knee osteotomy is generally considered for active patients who have arthritis in just one part of the knee, good range of motion, and a healthy body weight. It is most commonly used to treat medial (inner) compartment osteoarthritis in patients with a bow-legged (varus) alignment. Dr George Awwad offers knee osteotomy as part of a tailored joint preservation plan, taking into account each patient’s symptoms, lifestyle, goals, and imaging results.
Types of knee osteotomy: high tibial vs distal femoral
There are two main types of knee osteotomy procedures, each targeting a different bone depending on the direction of joint misalignment:
High Tibial Osteotomy (HTO)
A high tibial osteotomy involves cutting and reshaping the upper part of the tibia (shinbone). It is most commonly used in patients with varus deformity, where the knees are bowed outward and excess pressure is placed on the inner (medial) compartment of the knee. HTO works by shifting the body’s weight toward the less affected outer (lateral) part of the knee joint, aiming to reduce pain, improve function, and delay the progression of medial compartment osteoarthritis. This is the most common type of osteotomy performed for knee joint preservation.
Distal Femoral Osteotomy (DFO)
When is a knee osteotomy surgery typically recommended?
Unicompartmental (partial) knee arthritis
Malalignment of the knee joint
Young or active individuals
Knee pain that worsens with activity
If symptoms like pain, stiffness, or swelling are affecting your ability to participate in work, sport, or daily tasks and these symptoms are linked to joint malalignment or isolated arthritis, osteotomy may be part of a joint preservation strategy.
Preserved knee motion and cartilage in other compartments
Who might be a suitable candidate for knee osteotomy surgery?
Knee osteotomy is typically considered for patients who have specific characteristics that make them better suited to this joint-preserving approach rather than knee replacement surgery. It is not a universal solution for all knee arthritis, and careful assessment is essential.
Younger and active individuals
Isolated compartment osteoarthritis
Correctable knee alignment (varus or valgus)
Preserved range of motion and healthy surrounding cartilage
Healthy bone quality
Realistic expectations and commitment to rehabilitation
Who may not be suitable for a knee osteotomy?
Advanced, multi-compartment arthritis
Severe stiffness or limited range of motion
Inflammatory arthritis or systemic joint disease
Poor bone quality
Obesity
Smokers
Unrealistic expectations
Knee osteotomy vs partial vs total knee replacement: what’s the difference?
If you are living with knee pain caused by arthritis or joint damage, there are several surgical treatment options available. The most appropriate approach depends on the severity, location, and pattern of joint wear, as well as your age, activity level, and treatment goals. Below is a comparison of knee osteotomy, partial knee replacement, and total knee replacement.
Knee Osteotomy
A knee osteotomy involves reshaping or realigning the bones of the leg to offload pressure from the damaged part of the knee joint. It is typically recommended for younger or active patients who have arthritis affecting only one side (compartment) of the knee:
- Best suited for: Isolated medial or lateral compartment arthritis in younger, active individuals.
- Goal: To preserve the natural joint, reduce pain, and delay the need for knee replacement.
- Advantages: Retains native joint surfaces, may allow return to higher-impact activities.
- Considerations: Longer bone healing time; less suitable for advanced arthritis.
Partial Knee Replacement
Partial knee replacement (unicompartmental arthroplasty) involves replacing only the damaged compartment of the knee with a prosthetic implant. The rest of the joint, including the ligaments and cartilage in the unaffected areas, is preserved.
- Best suited for: Patients with moderate arthritis confined to one compartment, and good ligament function.
- Goal: To relieve pain while maintaining more natural joint movement.
- Advantages: Smaller incision, quicker recovery, retains more natural function.
- Considerations: Not appropriate for widespread arthritis or instability; risk of progression in other compartments.
Total Knee Replacement
Total knee replacement (arthroplasty) involves removing damaged cartilage and bone from the entire joint and replacing them with artificial components that resurface the femur, tibia, and sometimes the patella.
- Best suited for: Patients with severe, multi-compartment arthritis that limits mobility and quality of life.
- Goal: To provide long-term pain relief and restore function across the whole joint.
- Advantages: High success rate for pain relief and improved mobility.
- Considerations: Recovery time may be longer; joint mechanics may feel less natural than with native tissue.
Choosing the Right Approach
Dr George Awwad will perform a detailed clinical evaluation and review imaging to help determine which treatment aligns best with your symptoms, anatomy, and long term goals. Not every patient is suited to every procedure, and understanding the differences can help guide shared decision making.
Your knee osteotomy journey with Dr George Awwad: step by step
1. Initial Consultation and Assessment
- You will discuss your symptoms, lifestyle, and treatment goals.
- Dr Awwad will perform a physical examination of your knee.
- X-rays and other imaging (e.g. long-leg alignment films or MRI) will be reviewed to assess the joint surfaces and leg alignment.
- Based on this assessment, Dr Awwad will determine whether a knee osteotomy may be suitable for your condition.
2. Preoperative Planning
- Develop a personalised surgical plan based on your imaging and anatomy.
- Determine the appropriate type of osteotomy (e.g. high tibial or distal femoral) and calculate the exact degree of correction needed.
- Discuss the procedure with you in detail, including expected benefits, risks, and alternatives.
- Provide guidance on optimising your health before surgery, such as smoking cessation, managing chronic conditions, or strengthening the surrounding muscles through physiotherapy.
3. Admission and Anaesthesia
- You will be admitted to hospital and meet the anaesthetic team.
- Most knee osteotomies are performed under general anaesthetic, sometimes combined with a regional block for pain relief.
- You will be monitored closely throughout your admission to ensure comfort and safety.
4. The Surgical Procedure
- A small cut is made to access the tibia or femur, depending on the planned correction.
- A carefully measured wedge of bone is either removed (closing wedge) or created (opening wedge).
- The bone is realigned to redistribute load away from the worn part of the knee.
- The new alignment is secured with a specialised plate and screws.
- Bone graft or synthetic material may be used to support healing if needed.
5. Recovery in Hospital
- You may stay in hospital for 1–2 nights depending on your recovery and mobility.
- Pain is managed with medications and ice therapy.
- A physiotherapist will assist with gentle movement, walking, and early exercises.
- You will usually begin partial weight-bearing with crutches soon after surgery.
6. Rehabilitation at Home
- You will continue physiotherapy to gradually restore strength, mobility, and function.
- Dr Awwad will advise when to increase weight-bearing based on your progress and X-ray results.
- Most patients use crutches or a walking aid for 4–6 weeks.
- Regular follow-up appointments will be scheduled to monitor healing.
7. Return to Activities
- Driving may resume after 4–6 weeks when you can safely control the vehicle.
- Return to office-based work is often possible after 2–4 weeks.
- More physically demanding jobs may require a longer break.
- Low-impact exercise can usually begin around 3 months, with return to sport sometimes taking 6–12 months.
8. Long-Term Monitoring
What is the recovery process after knee osteotomy?
Hospital stay and immediate post-operative care
- Most patients remain in hospital for 1–2 nights following surgery.
- Pain is managed using oral medications and localised therapies like ice and elevation.
- A physiotherapist will assist you with early mobilisation, including:
- Bed exercises
- Sitting and standing transfers
- Walking with crutches or a frame
- A brace or support may be applied depending on the surgical technique used.
Weight-bearing and mobility milestones
- Weight-bearing is usually restricted initially to allow the bone to heal in its corrected position.
- Partial weight-bearing (with crutches or a walker) may be advised for the first 4 to 6 weeks, gradually increasing based on X-ray confirmation of bone healing.
- Most patients can begin full weight-bearing by 6–8 weeks, although this varies depending on:
- Whether a wedge was opened or closed
- Whether bone graft or synthetic material was used
- Your overall health and bone quality
Physiotherapy and rehabilitation
- A structured physiotherapy program plays a key role in your recovery and includes:
- Gentle range of motion exercises in the early weeks
- Gradual muscle strengthening of the quadriceps, hamstrings, and calf
- Balance and gait retraining
- Activity-specific exercises once weight-bearing improves
- Physiotherapy typically begins in hospital and continues after discharge through outpatient or home-based care.
Return to daily activities
| Activity | Activity Typical Timeline (guidance only) |
|---|---|
| Driving | 4–6 weeks (once able to control vehicle safely) |
| Office-based work | 2–4 weeks |
| Manual work | 8–12+ weeks |
| Low-impact activities | 3 months |
| High-impact sport | 6–12 months (depending on recovery and surgeon advice) |
Monitoring your progress
- Healing of the osteotomy site on X-ray
- Progress in physiotherapy
- Restoration of alignment and function
- Any signs of complications
You’ll be encouraged to keep up with physiotherapy, stay mobile, and gradually increase your activity level under guidance. Full recovery may take several months, but many patients experience significant relief of symptoms and improved function.
What are the potential risks or complications of knee osteotomy surgery?
General surgical risks
As with any surgery, some general risks apply, including:
- Infection at the surgical site
- Bleeding or the formation of a haematoma
- Deep vein thrombosis (DVT) or blood clots in the leg
- Adverse reaction to anaesthesia
These risks are typically low and are managed through preventative strategies such as antibiotics, blood thinners, and early mobilisation.
Specific risks associated with knee osteotomy
Non-union or delayed union
Loss of correction
Over-correction or under-correction
Nerve or blood vessel injury
Residual pain or stiffness
Compartment syndrome
Hardware irritation or removal
Long-term considerations
- Conversion to knee replacement: If arthritis progresses or symptoms return, a total or partial knee replacement may be needed later in life. A well-executed osteotomy can often delay this need.
- Leg length difference: Minor discrepancies in leg length may occur depending on the amount and type of bone correction.
Monitoring and prevention
Knee Osteotomy FAQs
How does knee alignment affect joint loading?
How is the bone realigned and stabilised in the procedure?
When can I return to work, driving, and sport after a knee osteotomy?
- Return to work: Most people can return to office-based work within 4–6 weeks, but more physically demanding roles may require 3 months or longer.
- Driving: You may resume driving once you have good control of your leg and are no longer reliant on strong pain medications—typically 6–8 weeks post-op.
- Sports and high-impact activity: These are usually resumed 6–9 months after surgery, depending on your recovery and rehabilitation progress.
What role does physiotherapy play in recovery?
- Strengthen the surrounding muscles
- Improve joint mobility and flexibility
- Support safe and gradual return to walking and daily activities
- Minimise the risk of post-operative complications, such as stiffness or weakness
