Direct Anterior Approach Total Hip Replacement
A muscle-sparing technique that may support faster recovery and improved mobility
Hip replacement surgery has transformed dramatically since its introduction in the 1960s. Early procedures were highly invasive, requiring large incisions and significant disruption to muscle and soft tissue to access the hip joint. While these techniques were often successful in relieving pain caused by arthritis or injury, they were associated with extended hospital stays, long recovery periods, and limited implant longevity.
Over time, advances in surgical technique, implant design, and peri-operative care have significantly improved the safety and effectiveness of hip replacement. The development of better prosthetic materials such as highly cross-linked polyethylene and modern ceramics has contributed to greater implant durability, with many joint replacements now lasting 20 years or more. Another major evolution has been in the way surgeons approach the hip joint. Traditional approaches, including the posterior and lateral methods, require cutting through muscles and tendons to reach the hip. While these remain widely used and effective in many cases, the desire to reduce tissue trauma and speed up recovery led to the emergence of minimally invasive techniques.
One of the most significant of these is the direct anterior approach, which uses a natural anatomical interval between muscle groups to access the joint. Unlike earlier so-called “minimally invasive” methods that only reduced the size of the skin incision but still involved cutting muscle, the anterior approach preserves key muscle structures. This has the potential to reduce pain, limit post-operative restrictions, and accelerate rehabilitation.
The evolution of hip replacement surgery continues to be supported by modern technologies such as pre-operative planning software, intraoperative imaging, robotic-assisted systems, and enhanced recovery protocols. These tools are helping surgeons like Dr George Awwad tailor each procedure to the individual patient, aiming for precise implant positioning, reduced complication risk, and more predictable outcomes.
Introduction to the Direct Anterior Approach
The direct anterior approach (DAA) is a modern surgical technique used in total hip replacement that allows Dr Awwad to reach the hip joint through a natural space between muscles, rather than cutting through them. This approach is sometimes referred to as muscle-sparing because the surrounding muscles and tendons are gently moved aside instead of being detached. By preserving soft tissues, patients may experience a smoother recovery and return to function compared to some traditional methods.
Over recent decades, hip replacement surgery has evolved considerably. While the operation has long been one of the most effective treatments for severe hip arthritis, improvements in surgical techniques, implant design, and imaging technology have made the procedure safer and more tailored to individual patients. Among these advances, the direct anterior approach has become increasingly popular because it combines proven outcomes of hip replacement with a less invasive pathway to the joint.
For many patients, the direct anterior approach can mean a smaller incision at the front of the hip, potentially reduced post-operative discomfort, and earlier mobility. Importantly, the technique is not suitable for everyone, and the decision about which surgical approach to use is made after a careful assessment of your hip condition, anatomy, lifestyle, and overall health.
Dr George Awwad offers hip replacement surgery using the direct anterior approach, supported by personalised surgical planning and detailed rehabilitation programs. During your consultation, he will discuss whether this approach is appropriate for you and provide tailored advice about your treatment and recovery.
Conventional approaches vs the anterior approach
Conventional approaches: posterior, lateral, and anterolateral
Lateral or Anterolateral Approach

Posterior Approach


The Anterior Approach: a muscle-sparing alternative
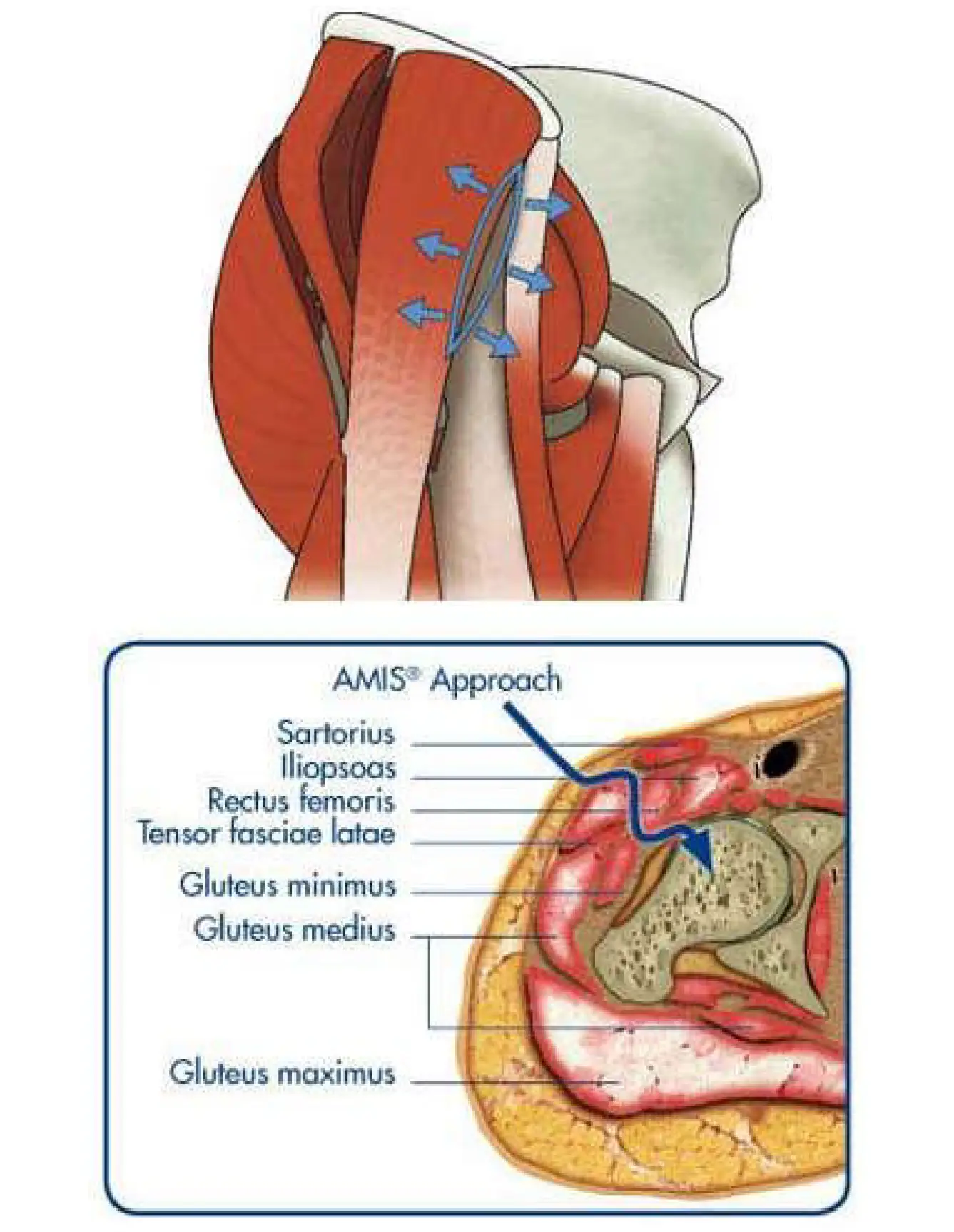
The direct anterior approach (DAA/AMIS) offers a modern alternative that aims to reduce tissue trauma. Unlike the posterior or lateral approaches, the anterior approach accesses the hip joint by working between natural muscular planes at the front of the hip.
- No muscles are cut to reach the hip joint
- Key muscle groups such as the gluteus medius, gluteus maximus, and external rotators are preserved
- Tendons and nerves are respected and retracted, not detached
This muscle-sparing technique is the foundation of AMIS® (Anterior Minimally Invasive Surgery), a method that may support a faster and less painful recovery compared to traditional techniques. Because muscles remain intact, many patients experience earlier return to walking, reduced need for postoperative precautions, and potentially a lower risk of hip dislocation.
Technologies that support the anterior approach

Specialised Anterior Approach Tables

Fluoroscopy and Intraoperative Imaging

Patient-Specific Preoperative Planning

Modern Prosthetic Implants
Today’s implants are designed to better mimic the natural function and biomechanics of the hip. Dr Awwad uses contemporary prosthetic designs that are well-suited to the anterior approach, including options that aim to reduce wear, increase stability, and accommodate the patient’s lifestyle and activity level.

Minimally Invasive Instrumentation

Other Minimally Invasive Options
- Mini-posterior approach: A smaller version of the traditional posterior approach, which uses a shorter incision but still involves muscle detachment.
- Two-incision technique: A rarely used method involving two small incisions, which may be associated with a steeper learning curve and higher complication risk.
- Anterolateral approach: Performed with a smaller incision but may still involve splitting or detaching certain muscle groups.
Why Dr Awwad Prefers the Anterior Approach
Who is a candidate for anterior approach hip replacement?
Potentially suitable candidates
- Those seeking faster functional recovery: The muscle-sparing nature of the anterior approach may support a shorter hospital stay, reduced post-operative pain, and quicker return to normal activities.
- Patients with a healthy body mass index (BMI): Patients with a lower BMI often benefit more easily from the minimally invasive incision and positioning required in the anterior approach.
- Younger or more active individuals: Patients who are motivated to return to an active lifestyle, including work or recreational activity, may appreciate the recovery profile of this approach.
- First-time hip replacements: The anterior approach is generally used for primary (first-time) total hip replacements rather than revision procedures.
When it may not be recommended
- Complex or revision hip replacements
- Significant obesity
- Unusual bone anatomy
- Previous incisions or surgeries that compromise the anterior soft tissues
In these situations, Dr Awwad may recommend an alternative approach to ensure the highest degree of safety and long-term function.
Every patient is different. Dr Awwad will conduct a thorough clinical assessment, review your imaging, and discuss your goals to determine whether the anterior approach is appropriate for you. If you are a suitable candidate, he will explain the surgical technique and expected recovery in detail, so you can make a confident and informed decision.
The surgical procedure: What to expect
Hospital admission and anaesthesia
Surgical positioning and incision
Joint access and preparation
- The damaged femoral head (ball of the hip joint) is removed.
- The acetabulum (hip socket) is carefully cleaned and shaped to fit the implant.
- A cup implant is inserted into the acetabulum, often with a polyethylene or ceramic liner.
- The femoral canal is then prepared to receive the stem component, which is inserted into the thigh bone.
- A femoral head is placed on the stem and fitted into the new socket.
Closure and dressing
- The soft tissues are allowed to return to their original positions.
- The incision is closed in layers using absorbable sutures.
- A sterile dressing is applied, and the leg is positioned for recovery.
Procedure duration
Post-operative care
Precautions after anterior approach hip surgery

Fewer restrictions, but still take care
Safe movement after surgery
- Use walking aids (such as crutches or a walking frame) as advised
- Avoid sudden twisting or pivoting on your operated leg
- Take care when getting in and out of cars or bed
- Avoid high-impact activities or uneven surfaces
Sitting and sleeping positions
- Choose chairs with firm support and armrests
- Avoid deep lounges or low sofas early on
- Sleep on your back or non-operated side with a pillow between your knees (unless advised otherwise)
Wound care and hygiene
- Keep the dressing clean and dry
- Avoid soaking the wound (no baths or swimming) until cleared by your surgeon
- Notify your care team if you notice redness, swelling, fluid leakage, or increased pain
When to resume activities
- Driving may be possible around 2–6 weeks after surgery (when walking confidently and no longer taking strong pain medications)
- Work may be resumed within 2–6 weeks, depending on the physical demands of your job
- Low-impact activities such as walking, swimming, and cycling are encouraged after your surgeon gives clearance
Exercises and physiotherapy after anterior approach THR

Early in-hospital rehabilitation
- Day of surgery or next morning: You will usually stand with assistance and begin walking short distances using a frame or crutches.
- Physiotherapist guidance: Hospital physiotherapists will teach you safe techniques for walking, getting out of bed, climbing stairs, and completing basic tasks.
At-home exercises
- Ankle pumps and circles – to promote circulation
- Gluteal squeezes – to activate hip muscles
- Quadriceps contractions – to build thigh strength
- Heel slides – to gently improve hip flexion
- Hip abduction (side leg lifts) – if approved by your surgeon
Progressive strengthening and mobility
- Weight-bearing and balance exercises
- Resistance band training for hip and core muscles
- Stationary cycling or low-impact cardio
- Gait retraining to improve walking mechanics
Returning to activity
- Driving may resume once you can confidently control the vehicle (usually 2–4 weeks).
- Work may be resumed within 2–6 weeks depending on your occupation.
- Low-impact sports such as swimming, cycling, or golf may resume in 6–12 weeks.
- High-impact activities such as running or contact sports are typically not advised.
Frequently asked questions about the anterior approach
Is the anterior approach truly “minimally invasive”?
How large is the incision for anterior hip replacement?
The incision is typically between 8 to 10 cm and may be smaller for patients with a slender build.
Will my muscles be cut during surgery?
Unlike other approaches (posterior or lateral), the anterior approach works between muscle groups rather than through them. This muscle-sparing technique reduces trauma to the tissues and may help preserve strength and stability in the hip.
Is robotic or computer navigation used during the anterior approach?
Yes, anterior approach hip replacement can be performed with the support of advanced navigation technologies. Dr Awwad uses modern planning software and intra-operative tools to help guide implant positioning and alignment.
What is the risk of dislocation with the anterior approach?
Dislocation risk is generally lower with the anterior approach compared to the posterior approach, due to preservation of key stabilising muscles. However, no approach is risk-free, and all patients receive guidance on precautions during recovery.
Is the anterior approach suitable for revision surgery?
In most cases, revision hip surgery is performed using other approaches, such as the posterior or lateral approach. The anterior technique is more commonly used for primary hip replacements in suitable candidates.
Is recovery faster with the anterior approach?
Many patients experience faster early recovery and mobilisation. You may walk the same day as surgery, return home earlier, and progress through physiotherapy more quickly than with other approaches. However, long-term outcomes are comparable once fully healed.
Are there any downsides or challenges with the anterior approach?
The anterior approach is more technically demanding for the surgeon and may carry a slightly higher risk of nerve irritation near the front of the hip. Careful patient selection and surgical experience are important factors in achieving good outcomes.
