Total Knee Replacement Surgery

A surgical option for relieving chronic knee pain and restoring joint function
Total knee replacement, also known as total knee arthroplasty, is a surgical procedure designed to relieve persistent knee pain and stiffness caused by severe arthritis, injury, or joint degeneration. When non-surgical treatments such as physiotherapy, medications, or corticosteroid injections no longer provide adequate relief, replacing the damaged knee joint with a prosthetic implant may help improve mobility and quality of life.
Dr George Awwad performs knee replacement surgery using modern techniques, including robotic-assisted surgery, kinematic alignment, and patient-specific pre-operative planning. Whether a full or partial knee replacement is recommended, his focus is on achieving precise, personalised outcomes that support a smoother recovery and long-term joint function.
When is knee replacement surgery recommended?
Total knee replacement surgery, also known as knee arthroplasty, may be recommended when non-surgical treatments no longer provide adequate relief from pain, stiffness, or loss of mobility caused by advanced knee joint damage. This procedure is most commonly considered for patients with severe osteoarthritis, rheumatoid arthritis, or post-traumatic arthritis that significantly impacts daily activities such as walking, climbing stairs, or sleeping comfortably.
- Ongoing knee pain at rest or during movement
- Swelling, stiffness, or reduced range of motion
- Difficulty walking, getting out of chairs, or using stairs
- Poor response to physiotherapy, medications, joint injections, or lifestyle changes
- Changes in leg alignment (e.g. bow-legged or knock-kneed appearance)
What are the common symptoms of knee arthritis?
Common signs and symptoms include:
-
Knee pain that worsens with activity
You may notice discomfort during walking, climbing stairs, or standing for long periods. Pain can vary from a dull ache to sharper sensations, particularly after increased use. -
Stiffness, especially in the morning or after rest
Many people with knee arthritis find it difficult to bend or straighten the knee after periods of inactivity. This stiffness may improve slightly with gentle movement. -
Swelling and inflammation
The knee joint may appear swollen or feel warm to the touch. Swelling can fluctuate and often increases after activity. -
Grinding, clicking or cracking sounds
As the smooth cartilage deteriorates, the bones may begin to rub together, causing noises or a grinding sensation during movement (crepitus). -
Reduced range of motion
Simple tasks such as bending down, squatting, or fully straightening the leg may become difficult. -
Weakness or instability
The knee may feel as though it is giving way or unable to support your body weight properly, which can make walking or standing challenging. -
Changes in leg alignment
Over time, arthritis may contribute to changes in how your knee looks or functions. This may include bow-legged (varus) or knock-kneed (valgus) alignment.

When to seek help
Am I a candidate for total knee replacement surgery?
-
Non-surgical treatments are no longer effective
Options such as physiotherapy, anti-inflammatory medications, weight management, and joint injections may offer short-term relief. However, if these approaches fail to control pain or maintain function, surgery may be the next step. -
You experience severe knee pain or stiffness
If your knee pain limits your ability to perform regular tasks like walking, climbing stairs, or getting out of a chair, or if stiffness makes movement difficult even after rest, it may be a sign of advanced joint damage. -
Imaging confirms significant joint degeneration
X-rays or other scans may show loss of cartilage, narrowing of the joint space, or bone-on-bone contact. These findings, in conjunction with your symptoms, help guide surgical decision-making. -
Your mobility and independence are affected
Many people consider knee replacement when pain or limited movement prevents them from participating in activities they enjoy, or when they rely on mobility aids to get around. -
Your symptoms are affecting your sleep or quality of life
Ongoing discomfort, sleep disruption, or emotional distress related to joint pain can all contribute to the decision to pursue surgical treatment.
Personalised decision making with Dr George Awwad
Dr Awwad takes a patient-centred approach to knee replacement surgery. During your consultation, he will assess your knee function, review imaging, and discuss your overall health, goals, and lifestyle. If surgery is appropriate, he will develop a personalised surgical plan tailored to your anatomy and specific needs, using advanced techniques such as robotic-assisted surgery and kinematic alignment where suitable.
Not every patient with knee arthritis will require surgery, and not everyone is a suitable candidate. Dr Awwad will guide you through your options, ensuring you understand the potential benefits, risks, and recovery involved so you can make an informed decision.
Who may not be suitable for knee replacement surgery?
Medical factors that may affect suitability
-
Uncontrolled medical conditions
If you have poorly managed diabetes, heart disease, lung conditions, or other serious illnesses, the risk of surgical complications may be higher. Optimising these conditions is often necessary before proceeding with surgery. -
Active infection
Any ongoing infection, whether in the joint or elsewhere in the body, must be treated and fully resolved prior to knee replacement. Surgery in the presence of infection significantly increases the risk of prosthetic joint infection, a serious complication. -
Severe vascular disease
Poor blood flow to the lower limbs may affect healing and increase the chance of wound-related complications after surgery. -
Skin problems around the knee
Open wounds, ulcers, or skin infections near the surgical site can increase the risk of post-operative infection and may delay surgery until resolved.
Lifestyle and other considerations
-
Significant obesity
While many people with higher body weight undergo successful knee replacement, severe obesity can increase the risk of complications such as wound healing problems, infection, or implant wear. Weight loss may be recommended before surgery. -
Poor bone quality or deformity
In some cases, bone loss, previous fractures, or severe joint deformity may require alternative surgical planning or specialised implants. -
Unrealistic expectations or limited rehabilitation capacity
Patients who are unable or unwilling to participate in post-operative physiotherapy, or who have unrealistic expectations about surgical outcomes, may not benefit as much from surgery. A commitment to rehabilitation is essential for a good outcome. -
Ongoing substance use
Smoking, excessive alcohol consumption, or drug use can impair healing and increase the risk of complications. Reducing or quitting these habits may be necessary before surgery is considered.
Personalised evaluation with Dr George Awwad
What is the difference between a total knee replacement and a partial knee replacement?
Knee replacement surgery is not a one-size-fits-all procedure. Depending on the pattern and severity of arthritis in your knee, you may be a candidate for either a total knee replacement or a partial (unicompartmental) knee replacement. Understanding the difference between these two procedures can help you feel more informed when discussing your options with Dr George Awwad.
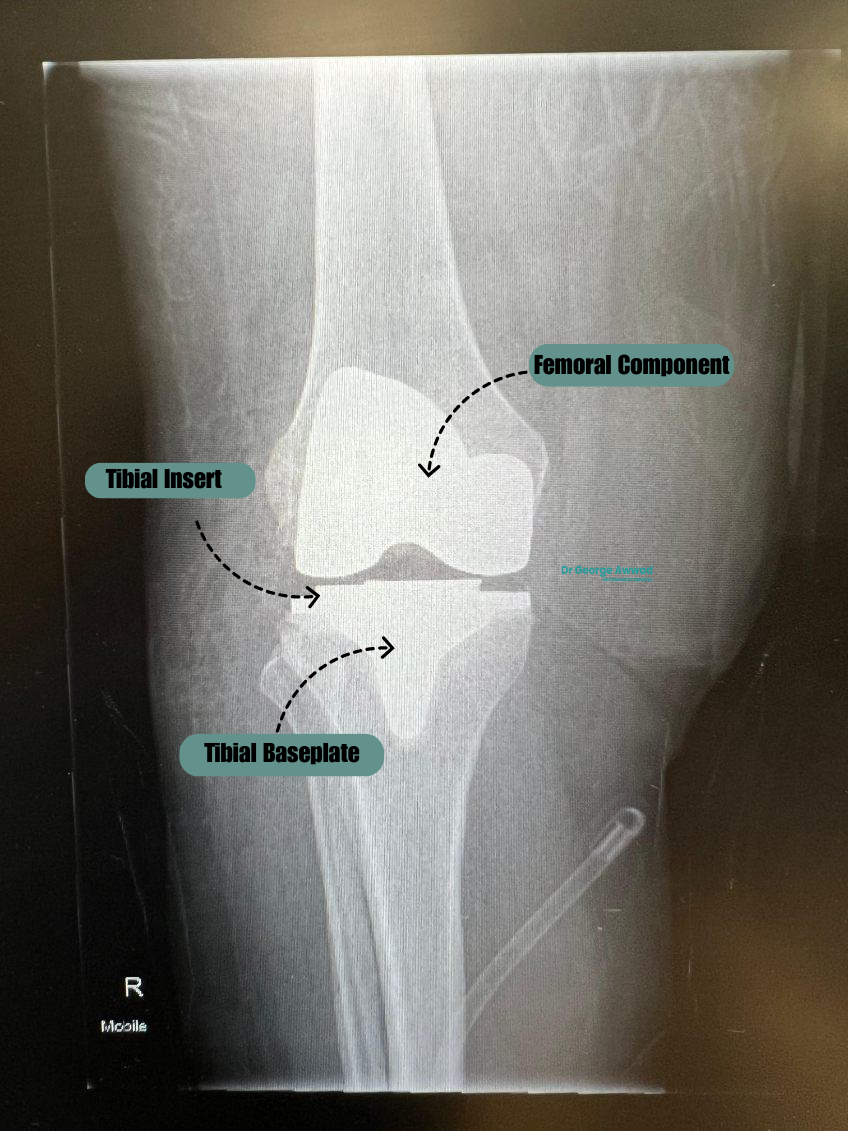
Total knee replacement (TKR)
In a total knee replacement, the worn-out surfaces of the knee joint are replaced with prosthetic components:
- Medial compartment (inside of the knee)
- Lateral compartment (outside of the knee)
- Patellofemoral compartment (under the kneecap) also often replaced but only when required
The procedure involves carefully removing damaged cartilage and bone and replacing them with metal and plastic implants that restore joint function. This is the most common form of knee replacement and is typically recommended when arthritis or degeneration affects the entire joint.
Key benefits of TKR:
- Comprehensive treatment for widespread arthritis
- Durable, long-lasting implant solutions
- Ability to address joint deformities and significant instability
Dr Awwad uses advanced surgical techniques such as robotic assistance and kinematic alignment to enhance precision and improve the natural feel and function of the replaced joint.
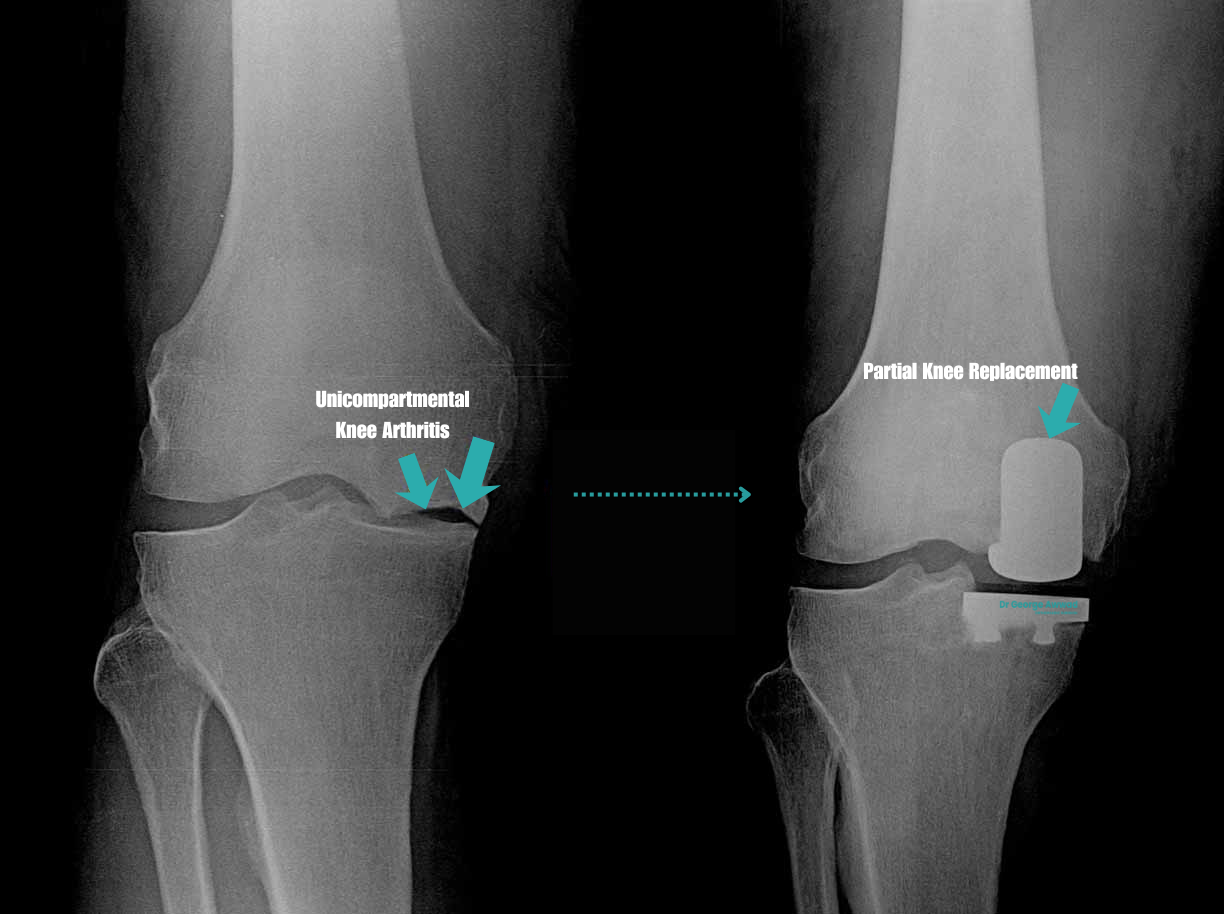
Partial knee replacement (PKR)
Partial knee replacement is a more limited procedure in which only the damaged compartment of the knee is resurfaced. The rest of the knee, including healthy cartilage, ligaments, and the other compartments is preserved.
This procedure may be suitable for patients with:
- Isolated medial or lateral compartment arthritis
- Intact anterior cruciate ligament (ACL)
- Well-preserved range of motion and knee alignment
Because only a portion of the joint is replaced, recovery is often quicker, and the knee may feel more “natural” after surgery.
Potential advantages of PKR:
- Smaller incision and less tissue disruption
- Faster recovery and rehabilitation
- Preservation of more natural knee mechanics
Not all patients however are suitable for this procedure. Dr Awwad will conduct a thorough clinical and imaging assessment to determine if you are a candidate.
How do robotic assisted surgery and kinematic alignment improve knee replacement?
Knee replacement surgery continues to evolve with advances in technology and surgical planning techniques. Two of the most significant developments in recent years are robotic-assisted surgery and kinematic alignment. These approaches aim to personalise the procedure for each patient, support more accurate implant positioning, make more precise cuts of the bone, and potentially enhance the overall outcome and recovery.
Robotic-assisted surgery: What is it and how does it help?
Robotic-assisted knee replacement involves the use of computer-guided systems to support the surgeon in planning and performing the procedure with a high level of precision. It does not mean the robot performs the surgery independently. Instead, Dr Awwad uses the robotic system as a tool to assist with accurate alignment, bone preparation, and implant placement based on your unique anatomy.
Benefits may include:
- Greater surgical precision by using real-time data and navigation
- Improved implant positioning, which may help with function and joint longevity
- Minimised soft tissue damage through tailored bone cuts and implant fit
- More consistent outcomes due to highly personalised surgical planning
Robotic systems can be used for both total knee replacement and partial knee replacement, depending on the patient’s condition and needs.

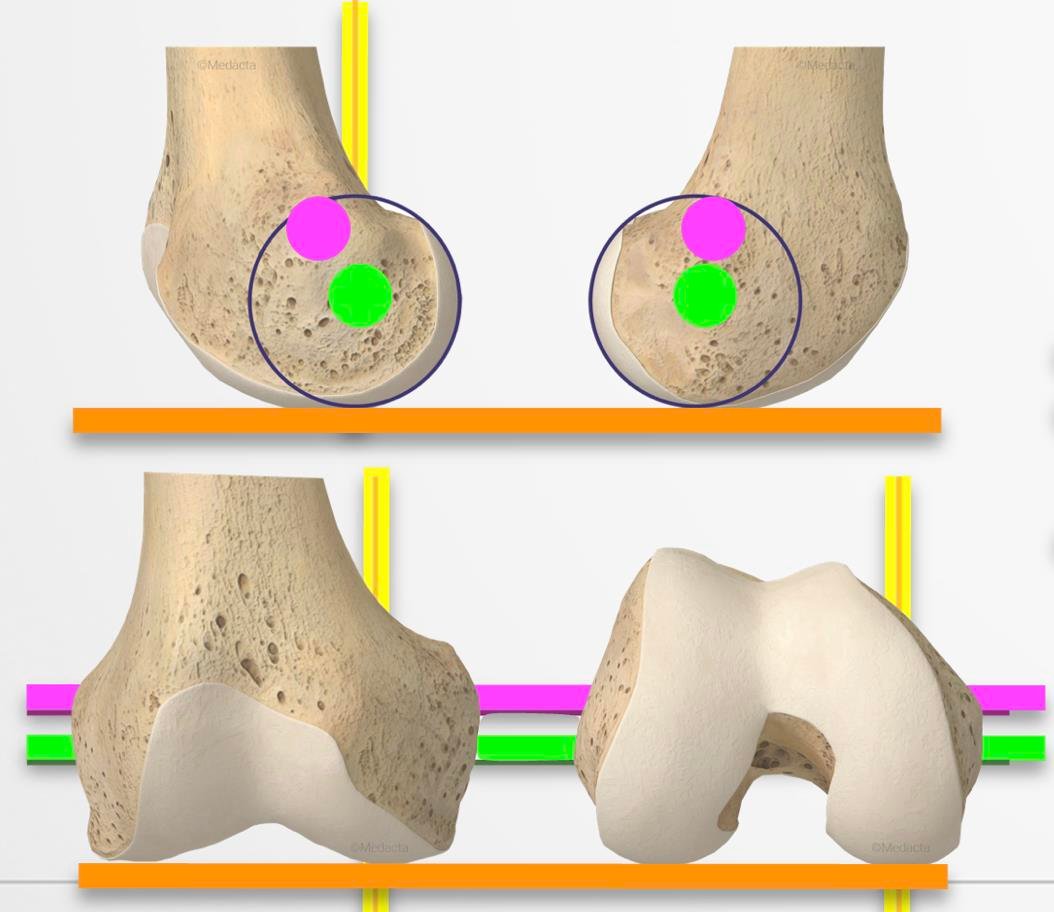
What is kinematic alignment and why is it important?
Traditional knee replacement surgery often uses a mechanical alignment technique, which places the implant in a neutral position relative to the body’s axis. While this method works well for many patients, it does not always match the natural alignment of an individual’s knee.
Kinematic alignment aims to restore the knee to its pre-arthritic position by closely matching the patient’s natural bone and joint lines. Instead of creating a standardised joint shape, the implant is positioned to mirror the original anatomy as much as possible.
Potential advantages of kinematic alignment include:
- A more natural-feeling knee joint after recovery
- Improved knee movement and flexibility
- Reduced need for ligament releases during surgery
- Increased patient satisfaction, particularly in everyday movements
This approach is carefully planned using pre-operative imaging and may be combined with robotic technology to further enhance precision.
Why Dr George Awwad incorporates these techniques
- Long-lasting, stable joint replacements
- Comfortable post-operative movement
- More rapid and confident return to daily activities
What role does imaging and a personalised surgical plan play in knee replacement?
Imaging: X-rays, CT scans, and 3D modelling
Your surgical journey begins with diagnostic imaging. Standard weight-bearing X-rays are usually the first step, helping to assess the degree of joint damage, alignment, and the condition of surrounding bone structures. In some cases, advanced imaging such as CT scans or MRIs may be used to build a more detailed picture of your knee.
Many modern knee replacement techniques now incorporate 3D imaging and modelling to support surgical planning. These images are used to evaluate the mechanical and kinematic alignment of your joint, and to understand how the bones, cartilage, and soft tissues move together. Accurate imaging provides the foundation for patient-specific alignment and implant positioning.
Personalised surgical planning
- Which type of implant best suits your joint
- The optimal alignment approach (mechanical or kinematic)
- The size and positioning of the prosthetic components
- Bone cuts and balancing techniques for ligaments and soft tissue
Integration with robotic-assisted surgery
Benefits for patients
- Improved accuracy of implant placement
- Better soft tissue balance and joint alignment
- Reduced risk of complications or early implant wear
- A more natural feeling knee after recovery
- Potential for quicker return to activity
What types of knee implants are used in total knee arthroplasty?
Main components of a knee replacement implant
- Femoral component – This metal piece caps the end of the thigh bone (femur) and may be curved to match the natural shape of the femur. It allows smooth movement against the tibial component.
- Tibial component – Placed on top of the shin bone (tibia), this component consists of a metal baseplate and a polyethylene (medical-grade plastic) insert that acts as a cushion and bearing surface.
- Patellar component – In some cases, the underside of the kneecap (patella) is also resurfaced with a polyethylene dome to improve joint tracking and movement.
Implant materials and design
Knee replacement implants are made from biocompatible materials that are designed to last many years. Common materials include:
- Cobalt-chrome or titanium alloy for strength and durability in the femoral and tibial components
- Highly cross-linked polyethylene for the insert, offering improved wear resistance
- Cemented or uncemented fixation options, depending on patient bone quality and other factors
Some implant designs may include:
- Posterior-stabilised designs for patients with weak or absent cruciate ligaments
- Cruciate-retaining designs that preserve the posterior cruciate ligament for more natural knee movement
- Medial-pivot or rotating platform designs to allow more natural joint kinematics in selected patients
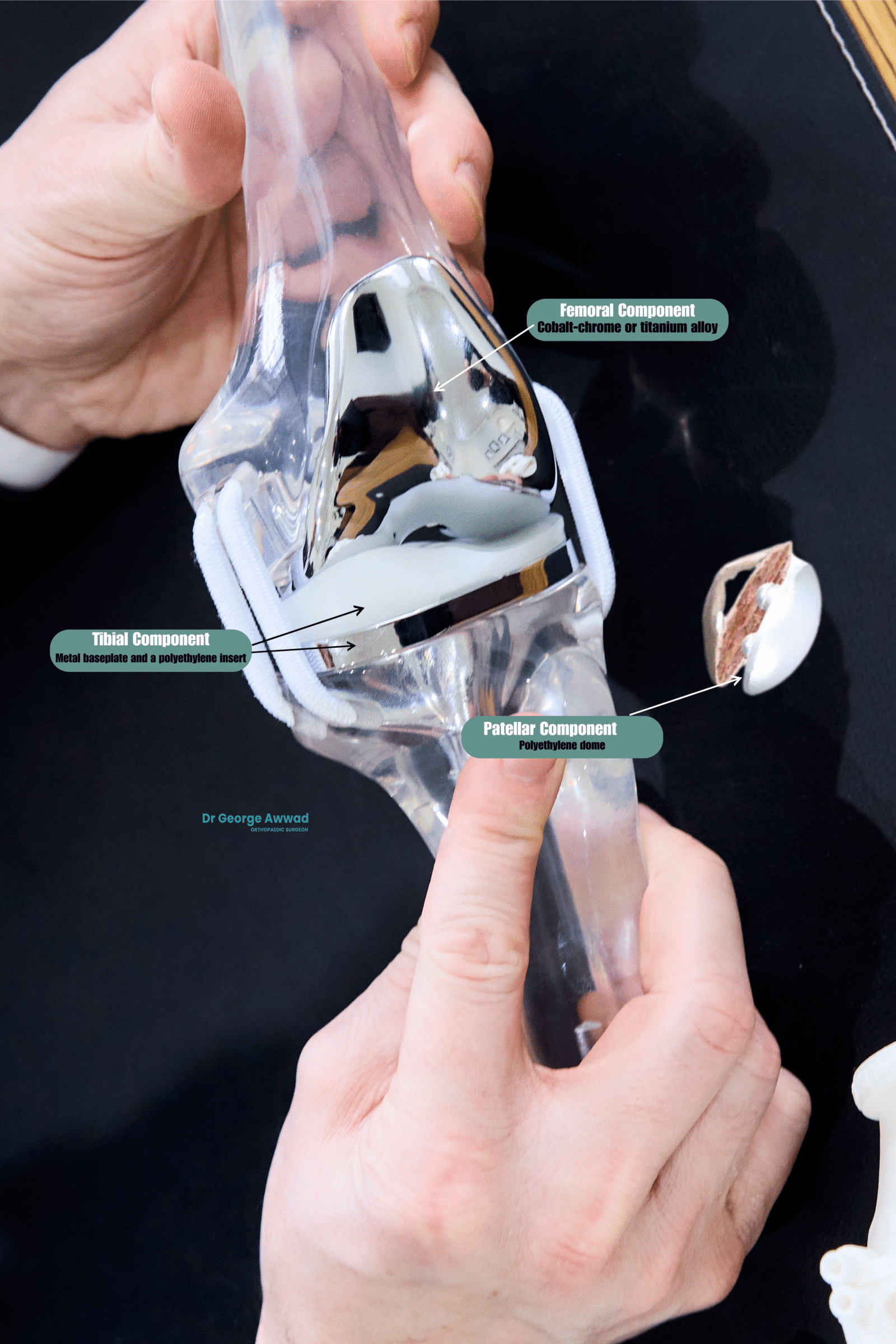
Customised implant selection
Dr Awwad takes a personalised approach to selecting your knee implant. A pre-operative imaging and planning process allows him to create a surgical plan tailored to your unique anatomy, ensuring that the chosen implant offers optimal alignment, fit, and function. Robotic assistance and kinematic alignment techniques may also support more accurate placement and balance of the implant.
Each patient’s implant choice is made with the goal of restoring joint stability, range of motion, and long-term durability, supporting you to return to daily activities with confidence.
What are the potential risks of knee replacement surgery?

Common risks of knee replacement surgery
Some of the more common risks include:
- Infection: This may occur in the wound or deeper around the implant. Strict sterile techniques and antibiotics are used to reduce this risk.
- Blood clots: Deep vein thrombosis (DVT) or pulmonary embolism (PE) can occur following surgery. Preventative measures such as blood-thinning medications, compression stockings, and early mobilisation are used to lower this risk.
- Bleeding or haematoma: Minor bleeding may occur around the surgical site. In rare cases, more significant bleeding may require intervention.
- Stiffness or reduced range of motion: Some patients may develop joint stiffness after surgery, which may require physiotherapy or additional procedures to improve movement.
- Implant loosening or wear: Over time, the implant may become loose or wear out, which could lead to the need for revision surgery. Modern implants are designed for durability, and proper alignment can reduce this risk.
- Persistent pain: A small percentage of patients may experience ongoing discomfort after surgery despite a technically successful procedure.
- Nerve or blood vessel injury: Although rare, nearby nerves or vessels can be injured during the operation, potentially causing numbness, weakness, or circulation issues.
- Allergic reactions: Some patients may have sensitivities or allergic reactions to the metals used in implants, though this is uncommon.
Risks specific to your health profile
Reducing your risk
- Minimally invasive approaches
- Robotic-assisted surgery
- Personalised pre-operative planning
- Enhanced recovery protocols
What are the benefits of total knee replacement surgery?
Relief from chronic knee pain
Improved mobility and joint function
Enhanced quality of life
Support for long-term joint function
Earlier recovery and rehabilitation
Using minimally invasive surgical techniques and enhanced recovery protocols, many patients can begin moving the knee within 24 hours of surgery. Early mobilisation, combined with tailored physiotherapy, helps promote circulation, reduce stiffness, and support a more structured recovery pathway.
Individualised care and planning
What does the knee replacement journey with Dr George Awwad involve?
Undergoing knee replacement surgery is a significant decision, and Dr George Awwad is committed to guiding you through each step with clarity, precision, and personalised care. From initial consultation to recovery and follow-up, your experience will be tailored to your unique needs and goals.
Initial Consultation and Clinical Assessment
Your journey begins with a thorough assessment. Dr Awwad will review your medical history, symptoms, previous treatments, and imaging (such as X-rays or MRI scans). He will examine your knee to assess range of motion, alignment, and strength, and discuss how your condition is affecting your quality of life. If surgery is appropriate, Dr Awwad will explain the options available, including whether total or partial knee replacement may be most suitable, and whether robotic-assisted techniques and kinematic alignment could support your outcome.
Advanced Imaging and Personalised Surgical Planning
Once a surgical decision is made, detailed imaging (such as 3D CT scans or weight-bearing X-rays) may be arranged to help create a customised surgical plan. These scans are used to generate a patient-specific model of your knee, allowing Dr Awwad to:
- Select the right implant size and type
- Optimise joint alignment and soft tissue balance
- lan precise bone cuts and implant positioning
This careful planning helps improve the predictability and accuracy of the procedure.
Pre-operative Preparation
You will receive guidance on how to prepare for surgery, including:
- Pre-operative blood tests or assessments
- Advice on medications and fasting instructions
- Information about anaesthetic options
- Enhanced recovery protocols, including physiotherapy planning
If necessary, Dr Awwad may coordinate care with your GP, physiotherapist, or anaesthetist to optimise your health before surgery.
Knee Replacement Surgery
Dr Awwad performs knee replacement surgery using advanced techniques, including robotic-assisted systems and muscle-sparing approaches where appropriate. Surgery takes place at one of his accredited private or public hospital locations. During the procedure:
- Damaged bone and cartilage are carefully removed
- The joint is reshaped to fit the implant components
- Robotic systems and alignment tools are used to ensure precision
- The prosthetic components are secured and the knee is tested for motion and stability
The procedure usually takes around 1 to 1.5 hours, and most patients remain in hospital for 2-3 nights depending on the surgical plan and recovery progress.
Post-operative Care and Pain Management
After surgery, pain management is a key focus. Dr Awwad works with your care team to ensure:
- Appropriate use of medications (including regional anaesthesia or nerve blocks)
- Early mobilisation, often beginning on the day of or after surgery
- Prevention of complications such as blood clots or infection
Rehabilitation and Follow-up
Physiotherapy begins shortly after surgery to support mobility, strength, and confidence. You will receive a tailored rehabilitation plan, with guidance on walking aids, exercises, and gradually increasing your activity. Follow-up appointments with Dr Awwad are scheduled to monitor your healing, check implant positioning via imaging, and answer any questions you may have during recovery.
Long-term Support
Even after you’ve returned to regular activity, ongoing monitoring may be recommended to check your implant and joint function. Dr Awwad remains available to support your recovery and address any new concerns should they arise.
What does the knee replacement journey with Dr George Awwad involve?
Undergoing knee replacement surgery is a significant decision, and Dr George Awwad is committed to guiding you through each step with clarity, precision, and personalised care. From initial consultation to recovery and follow-up, your experience will be tailored to your unique needs and goals.
Initial Consultation and Clinical Assessment
Advanced Imaging and Personalised Surgical Planning
- Select the right implant size and type
- Optimise joint alignment and soft tissue balance
- Plan precise bone cuts and implant positioning
Pre-operative Preparation
- Pre-operative blood tests or assessments
- Advice on medications and fasting instructions
- Information about anaesthetic options
- Enhanced recovery protocols, including physiotherapy planning
Knee Replacement Surgery
- Damaged bone and cartilage are carefully removed
- The joint is reshaped to fit the implant components
- Robotic systems and alignment tools are used to ensure precision
- The prosthetic components are secured and the knee is tested for motion and stability
Post-operative Care and Pain Management
- Appropriate use of medications (including regional anaesthesia or nerve blocks)
- Early mobilisation, often beginning on the day of or after surgery
- Prevention of complications such as blood clots or infection
Rehabilitation and Follow-up
Long-term Support
How is pain managed after knee replacement surgery?
Pre-operative Planning for Pain Relief
Anaesthetic Options During Surgery
- Spinal Anaesthesia: A common choice for knee replacement that provides pain relief during and immediately after the procedure.
- Regional Nerve Blocks: A peripheral nerve block (such as an adductor canal or femoral nerve block) may be used to numb the area around your knee while preserving muscle control.
- General Anaesthesia: Sometimes used in combination with other methods, depending on your needs.
Post-operative Pain Management Strategies
- Oral Medications: Such as paracetamol, anti-inflammatory drugs, and sometimes mild opioids to manage moderate pain.
- Cold Therapy: Icing or cold compression devices can help reduce swelling and provide natural pain relief.
- Activity Modification: Gradually resuming movement with physiotherapy while avoiding overexertion also supports comfort during recovery.
Minimising the Use of Strong Opioids
Enhanced Recovery Protocols
- Minimally invasive surgical techniques (where appropriate)
- Multi-modal pain relief
- Early mobilisation with physiotherapy support
What is the recovery timeline after knee replacement surgery?
Recovery following total knee replacement surgery is a gradual process that varies from person to person. Factors such as age, general health, the severity of knee arthritis, and your commitment to physiotherapy all play a role. Dr George Awwad will provide you with personalised guidance and support at every stage of your recovery to help you regain mobility and return to your daily activities safely.
Below is a general overview of what you may expect after surgery:
Day of Surgery
- You will usually begin moving your knee on the day of surgery or the next morning.
- Most patients stand and take a few steps with the assistance of a physiotherapist and walking aid.
- Pain is managed with a multi-modal strategy, allowing early movement without excessive discomfort.
Hospital Stay (1–3 Days)
- You will be assisted in walking short distances, using stairs, and completing basic self-care tasks.
- Physiotherapy sessions focus on improving knee flexibility, muscle strength, and safe mobility.
- Most patients are discharged home or to a rehabilitation facility within a few days, depending on progress.
First 2 Weeks Post-Surgery
- You’ll likely use crutches or a walker during this early period.
- Swelling, bruising, and stiffness are common but should gradually improve with rest, elevation, and exercises.
- Wound care is important, and your dressing will typically be changed during your post-operative check.
Weeks 3–6
- You’ll likely use crutches or a walker during this early period.
- Physiotherapy becomes more active, focusing on regaining range of motion, strength, and gait correction.
- Most patients can resume some light daily activities, but driving, work, and sports may still be limited.
Weeks 6–12
- You should notice a significant reduction in pain and stiffness.
- Walking, stair climbing, and low-impact exercises become easier.
- Many patients return to desk-based work around this time, although more physically demanding roles may take longer.
3–6 Months
- Knee strength and confidence in movement continue to improve.
- You may return to low-impact recreational activities such as cycling, swimming, or golf.
- Some swelling and stiffness may persist after prolonged activity but usually improve with time.
6–12 Months and Beyond
- Your knee may continue to feel stronger and more natural up to a year after surgery.
- Full recovery timelines vary, but most patients can expect long-term improvement in pain, mobility, and function.
- High-impact sports or activities involving sudden movements are generally discouraged to protect the implant.
What precautions should I follow after knee replacement surgery?
Protecting your new knee in the early stages
- Avoid sudden twisting or pivoting on the surgical knee.
- Use crutches or a walker as recommended to support your balance and prevent falls.
- Follow weight-bearing instructions provided by Dr Awwad or your physiotherapist. Some patients are allowed to fully weight-bear early, while others may be restricted initially depending on the complexity of surgery.
- Keep the wound clean and dry, and monitor for signs of infection such as redness, swelling, or fluid leakage.
- Elevate your leg and use ice packs to reduce swelling and discomfort.
Moving safely at home
- Remove trip hazards like rugs and cords from walkways.
- Install handrails in bathrooms and near stairs.
- Use a shower chair or non-slip mats if necessary.
- Avoid low chairs or deep couches that are difficult to get in and out of.
Medication and anticoagulant precautions
- Take medications exactly as instructed.
- Be aware of potential signs of deep vein thrombosis (DVT), such as calf pain or swelling.
- Inform your GP, dentist, or other treating doctors that you are on anticoagulants if you need other procedures or treatments during your recovery.
Activity modification
- Avoid high-impact activities such as running or jumping until cleared by your surgeon.
- Postpone driving until you are safely mobile and no longer taking strong pain medication—typically 4 to 6 weeks post-op depending on your recovery and which leg was operated on.
- Gradually build up your activity level with physiotherapy guidance.
When to contact Dr Awwad’s rooms
- Sudden increase in pain, swelling, or bruising
- Fever or chills
- Wound drainage, redness, or heat
- Difficulty breathing or chest pain (seek urgent medical attention)
How does physiotherapy support recovery after knee replacement?
Physiotherapy is an essential part of your recovery following total or partial knee replacement surgery. It plays a critical role in helping you regain strength, mobility, balance, and confidence as you return to daily activities.

Beginning rehabilitation early
- Improve circulation and reduce the risk of blood clots
- Begin activating the quadriceps and surrounding muscles
- Encourage safe movement, such as standing and short walks with a frame or crutches
- Prevent stiffness and maintain joint flexibility
Tailored home and outpatient rehabilitation
- Strengthening exercises for the quadriceps, hamstrings, and hip muscles
- Gait retraining to help you walk smoothly and evenly
- Balance and coordination activities to reduce the risk of falls
- Gradual progression to more complex movements, such as stair climbing or functional tasks
Supporting long-term outcomes
- Improve joint range of motion
- Support soft tissue healing and reduce post-operative swelling
- Enhance joint stability and muscle control
- Prevent compensation patterns or limping
- Support a safe and timely return to daily routines, work, or recreational activities
Working with your healthcare team
When can I return to normal activities after knee replacement?
The timeline for returning to normal activities after knee replacement surgery can vary depending on your overall health, the complexity of your surgery, and how your recovery progresses. While each patient’s journey is unique, the following guide provides general expectations.
In the first few days to weeks
- Safe walking and basic mobility
- Managing swelling and pain
- Beginning physiotherapy exercises
Returning to daily activities
- Self-care: Most people can independently manage dressing, showering, and other self-care activities within the first 2 to 4 weeks.
- Driving: You may be able to return to driving between 4 to 6 weeks, depending on which leg was operated on and your ability to safely control the vehicle.
- Work: Patients with desk-based jobs often return within 4 to 6 weeks. Roles involving standing, walking, or manual labour may require 8 weeks or longer.
- Low-impact exercise: Activities like walking, cycling on a stationary bike, and swimming (after wound healing) are generally encouraged after the first 4-6 weeks.
Long-term recovery and physical goals
- Walk longer distances without pain
- Return to recreational activities such as golf, cycling, or hiking
- Experience improved sleep and reduced need for pain medication
