Hip Fractures and Trauma

Understanding acute hip injuries and how they’re managed
Hip fractures and traumatic injuries to the hip joint can have a significant impact on your ability to move, weight-bear, and perform everyday activities. These injuries are particularly common in older adults following a fall, but they may also occur in younger people after high-impact trauma such as motor vehicle accidents or sporting injuries. Prompt diagnosis and appropriate treatment are essential to reduce complications and support a return to mobility. Management may involve surgical or non-surgical approaches, depending on the type, severity, and location of the injury.
Dr George Awwad provides timely assessment and tailored treatment for hip trauma, with a focus on restoring function, preventing long-term joint problems, and supporting rehabilitation.
What is a hip fracture or traumatic hip injury?
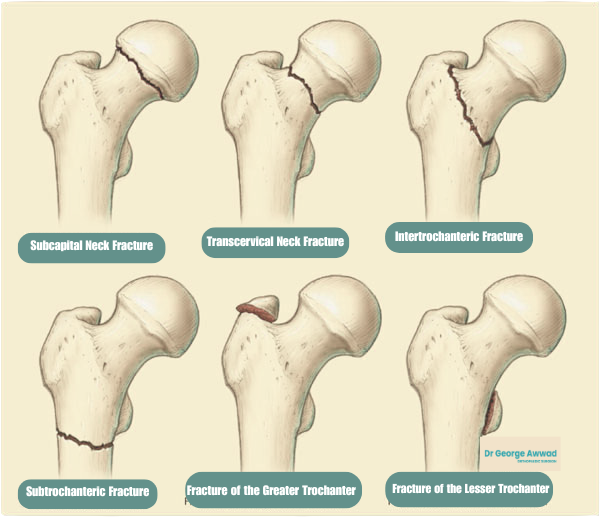
A hip fracture refers to a break in the upper part of the femur (thigh bone), near where it connects with the pelvis to form the hip joint. Most hip fractures occur just below the ball of the hip joint (the femoral head) and are typically classified based on their location and pattern.
Common types include:
- Femoral neck fractures – occur just below the ball of the hip
- Intertrochanteric fractures – occur slightly lower, between the neck and the shaft of the femur
- Subtrochanteric fractures – occur even lower on the femur, just below the trochanters
A traumatic hip injury refers more broadly to any injury that affects the bones, cartilage, ligaments, or muscles around the hip joint due to a high-impact event such as a fall, sports injury, or car accident. This can include dislocations, pelvic fractures involving the hip socket (acetabulum), or soft tissue injuries like tendon or labral tears.
Classification and severity
- Location of the fracture (e.g. femoral neck, intertrochanteric)
- Displacement (whether the bone fragments are still aligned or separated)
- Stability (how likely the fracture is to remain in place)
- Trauma mechanism (low-energy such as a fall, or high-energy such as a collision)
Common causes of hip fractures and trauma
Hip fractures and other traumatic hip injuries can result from a wide range of causes. These causes generally fall into two categories; low-energy injuries, which are more common in older adults, and high-energy injuries, which are more often seen in younger individuals.
1. Falls (especially in older adults)
- Reduced balance and coordination
- Muscle weakness
- Vision problems
- Use of walking aids or unsafe footwear
- Medications that cause dizziness or drowsiness
- Environmental hazards such as slippery floors or poor lighting
2. High-impact trauma (especially in younger people)
- Motor vehicle or motorcycle accidents
- Pedestrian-versus-car collisions
- Significant sporting injuries (e.g. contact sports, skiing, cycling crashes)
- Falls from height (e.g. ladder, horse, roof)
3. Stress fractures
Although less common, stress fractures of the hip can occur in athletes, military recruits, or people who perform repetitive weight-bearing activity. These small cracks in the bone are usually due to overuse or repetitive strain and can develop over time if rest and recovery are inadequate.
4. Pathological fractures
- Osteoporosis (most common)
- Metastatic cancer that has spread to the bone
- Infection in the bone (osteomyelitis)
- Benign bone cysts or tumours
Signs and symptoms to look out for
1. Sudden pain in the hip or groin
A hip fracture typically causes severe pain in the outer upper thigh or groin area. The pain may worsen with movement or when trying to bear weight. Even mild pain after a fall should be assessed, particularly in older adults.
2. Inability to stand or walk
People with a hip fracture are often unable to stand, walk, or put weight on the affected leg. If walking is still possible, it may be with a noticeable limp
Diagnosing a hip fracture
1. Clinical assessment
Dr Awwad will begin with a thorough history and physical examination. This includes asking about the mechanism of injury, such as a fall or direct trauma, and checking for pain, swelling, deformity, or inability to move the leg.
- Shortening or outward rotation of the leg
- Localised tenderness around the hip or groin
- Difficulty or inability to bear weight
2. Imaging tests
- X-rays: Usually the first step in diagnosis. X-rays can identify most fractures of the femoral neck, intertrochanteric region, or subtrochanteric area.
- MRI or CT scan: These may be used if X-rays are inconclusive or if further detail is needed. An MRI can detect stress fractures or occult fractures (not visible on X-ray), and a CT scan may help assess complex fracture patterns or joint involvement.
3. Additional assessments
In some cases, especially for older patients or those with osteoporosis, bone density tests (DEXA scans) may be recommended to assess underlying bone health and risk of future fractures.
Initial treatment and emergency care
A hip fracture or traumatic hip injury is a medical emergency that requires urgent assessment and treatment. Early stabilisation and hospital care are essential to minimise complications and improve outcomes—especially in older patients or those with other health conditions.
What to do if you suspect a hip fracture
- Keep the person still and warm.
- Do not attempt to move them unless they are in immediate danger.
- Reassure them and monitor for signs of shock (such as pale skin, rapid breathing, or confusion).
Assessment in the emergency department
- Pain relief: Strong analgesics or regional nerve blocks to manage severe discomfort.
- X-rays and scans: To confirm the fracture and determine the exact location and type of injury. CT or MRI scans may be used for more complex or subtle fractures.
- Blood tests and monitoring: To assess overall health, identify other injuries, and prepare for surgery if needed.
- Temporary limb support: A pillow, splint or foam wedge may be used to keep the leg stable and reduce pain until surgery.
Early planning for surgery and recovery
Early surgical intervention is often recommended, ideally within 24 to 48 hours. During this time:
- The orthopaedic team will assess the type of fracture and recommend the most appropriate surgical approach.
- Medical specialists (such as anaesthetists or geriatricians) may be involved to optimise health before surgery, especially for older patients with other medical conditions.
- You will also meet the nursing and allied health teams who will support your post-operative care and recovery.
Surgical treatment options for hip fractures
Surgery is often required to restore stability and mobility after a hip fracture. The type of operation recommended will depend on the location and severity of the fracture, the patient’s age, bone quality, pre-existing joint conditions (such as arthritis), and overall health.
Hip pinning or internal fixation (ORIF)
- For fractures that are well-aligned or minimally displaced, particularly in younger or more active individuals.
- Metal screws, rods, or plates are used to stabilise the broken bone fragments and allow them to heal in position. This procedure is known as open reduction and internal fixation (ORIF).
- Preserves the patient’s natural hip joint.
- May allow early mobilisation, depending on bone healing.
Hemiarthroplasty (Partial hip replacement)
- Commonly performed for displaced fractures of the femoral neck, particularly in older adults where bone healing may be compromised.
- The damaged femoral head (the “ball” of the hip joint) is removed and replaced with a prosthetic implant. The socket of the joint (acetabulum) is not replaced.
- Reduces the risk of complications like non-union or avascular necrosis.
- Often allows early weight-bearing after surgery.
Total hip replacement (Total hip arthroplasty)
- In selected patients who are active, relatively healthy, and have pre-existing arthritis or other joint damage.
- Both the femoral head and the acetabulum are replaced with prosthetic components. This may be performed using minimally invasive techniques in suitable candidates.
- Offers improved long-term function in selected patients.
- May reduce the risk of future joint problems compared to hemiarthroplasty.
Intramedullary nailing (for subtrochanteric and intertrochanteric fractures)
- For fractures that occur further down the femur, below the neck of the femur.
- A metal rod (nail) is inserted into the centre of the femur and secured with screws to stabilise the fracture.
- Provides strong internal support for healing.
- Provides strong internal support for healing. Minimally disruptive to surrounding tissues.
Dr George Awwad’s approach to hip fracture surgery
Dr Awwad provides individualised surgical treatment tailored to the specific type of hip fracture and the patient’s functional needs. His goal is to restore mobility as early as possible, while minimising the risk of complications such as implant failure, infection, or delayed healing. Where appropriate, minimally invasive or muscle-sparing techniques may be used to support faster recovery and rehabilitation.
Post-operative care and rehabilitation
Prompt medical attention is essential after a suspected hip fracture or traumatic hip injury.
If you or someone you are with experiences a sudden, painful hip injury, especially after a fall or accident, it is important to seek emergency care immediately. Early treatment can reduce complications and improve long-term outcomes.
- Initial assessment: The medical team will assess your condition, including checking for signs of shock, bleeding, or associated injuries. Vital signs, pain levels, and neurological function will be monitored.
- Imaging: An X-ray is typically the first imaging tool used to confirm a hip fracture. In some cases, a CT scan or MRI may be required to assess more complex or non-displaced fractures.
- Pain management: Pain relief is usually administered early, using medications such as oral analgesics or intravenous pain control, depending on severity.
- Stabilisation: In some cases, the hip may be immobilised or supported while awaiting surgical intervention. Pressure-relieving mattresses and nursing support help protect the affected limb.
Hospital admission is usually required for further management, which may include surgical repair, depending on the type and severity of the fracture.
Dr George Awwad works closely with emergency and hospital teams across Adelaide to coordinate timely surgical care for hip trauma patients. His approach prioritises patient safety, effective pain control, and early mobilisation to reduce the risk of complications.
Rehabilitation and long-term outcomes after hip fracture surgery?
Recovery after a hip fracture is a gradual process that requires coordinated care, physiotherapy, and ongoing support. The goal is to restore mobility, improve independence, and reduce the risk of complications or future falls.
Post-operative rehabilitation
- Prevent complications such as blood clots, pneumonia, or muscle wasting
- Promote healing and maintain strength in the uninjured limbs
- Restore confidence in walking and weight-bearing
- Hospital-based physiotherapy and occupational therapy
- Inpatient rehabilitation at a specialised facility
- Home-based rehabilitation programs
- Outpatient physiotherapy services
Long-term outlook and functional recovery
- Your pre-injury level of fitness and independence
- The type of fracture and surgical repair
- Co-existing medical conditions
- Your level of engagement in physiotherapy
Preventing future falls and fractures
- Bone health assessments to detect and manage osteoporosis
- Medication reviews to identify those that may affect balance
- Home safety assessments to eliminate trip hazards
- Strength and balance training with a physiotherapist
