Hip Bursitis
A common cause of outer hip pain caused by inflammation of the bursa over the greater trochanter
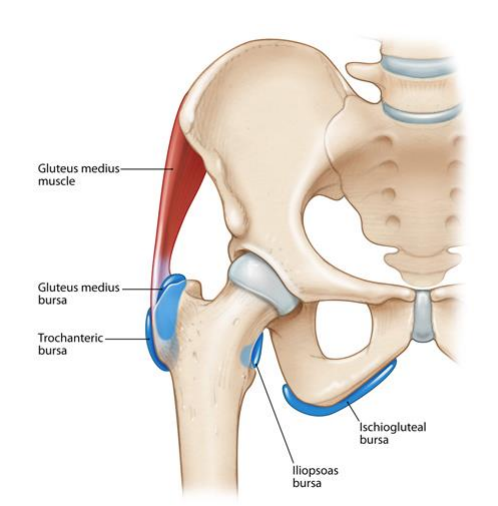
Hip bursitis, also referred to as trochanteric bursitis, is a condition where the bursa located over the bony prominence on the outer side of the hip (the greater trochanter) becomes inflamed. This inflammation can cause persistent pain and tenderness on the outside of the hip, often worsening with activity or when lying on the affected side.
While it frequently affects middle aged and older adults, hip bursitis is also seen in active individuals such as runners, footballers, and dancers, particularly due to repetitive strain or biomechanical stress on the hip. The bursae are small, fluid-filled sacs that reduce friction between bones, tendons, and muscles.
When they become irritated or overloaded, they can swell and become painful, a condition known as bursitis.
Understanding the underlying cause of your hip pain is essential. Dr George Awwad provides careful assessment, imaging where appropriate, and tailored treatment strategies to relieve discomfort and restore function.
What causes hip bursitis?
Hip bursitis, or trochanteric bursitis, occurs when the bursa over the outside of the hip becomes irritated and inflamed. This bursa normally acts as a cushion between the bony point of the hip (the greater trochanter) and the muscles and tendons that pass over it. When this cushioning structure is subjected to excessive friction or pressure, it can swell and become painful.
Common causes and contributing factors
-
Repetitive movements or overuse
Activities that involve repeated hip motions such as long-distance running, cycling, climbing stairs, or prolonged standing can cause microtrauma to the bursa and surrounding soft tissues. -
Direct trauma or falls
A blow to the outer hip, such as from a fall or bump against hard surfaces, can cause inflammation of the bursa. -
Hip muscle weakness or imbalance
Poor strength or coordination in the gluteal muscles can alter biomechanics, placing extra stress on the bursa. -
Leg length differences
A discrepancy in leg length can change how force is distributed across the hip during walking or running, increasing the risk of bursitis. -
Underlying hip or spine conditions
Conditions such as hip osteoarthritis, spinal arthritis, or scoliosis may contribute to abnormal movement patterns that irritate the bursa. -
Previous hip surgery or prosthesis
Patients who have had hip replacement surgery or other procedures may develop bursitis due to changes in soft tissue tension or altered gait. -
Rheumatoid arthritis or other inflammatory conditions
Systemic inflammatory disorders can increase the risk of bursitis in multiple joints, including the hip. -
Poor posture or biomechanics
Improper walking patterns, poor footwear, or incorrect training techniques may all contribute to bursa irritation.

Symptoms of hip bursitis
Hip bursitis typically presents as pain on the outside of the hip, often near the bony prominence called the greater trochanter. The discomfort may start as a dull ache and progressively worsen, especially with movement or pressure.
-
Pain over the outer hip
This is the hallmark symptom, often described as sharp or burning. It may radiate down the side of the thigh but usually does not extend below the knee. -
Tenderness to touch
Pressing on the outside of the hip may reproduce the pain. Many patients find lying on the affected side too uncomfortable. -
Pain with movement or activity
Walking, climbing stairs, standing for long periods, or getting up from a chair can aggravate symptoms. Athletes may notice increased pain during or after training sessions. -
Worsening pain at night
Discomfort often intensifies when lying on the affected side, making sleep difficult. -
Swelling or warmth (less common)
In some cases, inflammation of the bursa may result in mild swelling or warmth around the hip. -
Stiffness or reduced mobility
While hip joint range of motion is often preserved, pain may cause guarded movements or altered gait patterns.
How is hip bursitis diagnosed?
1. Medical history
- The location, nature, and severity of your pain
- Any recent injuries or overuse activities
- Whether certain positions (such as lying on your side) worsen your discomfort
- Your medical and activity history, including any repetitive strain or inflammatory conditions
2. Physical examination
- Palpate the outer hip to check for tenderness over the greater trochanter
- Assess your hip range of motion and strength
- Observe your gait and posture
- Reproduce the pain through specific clinical tests to confirm bursitis and rule out other causes such as tendinopathy or joint arthritis
3. Imaging studies (if needed)
- Ultrasound: A helpful tool to detect fluid in the bursa or signs of inflammation
- MRI: Can provide a more detailed view of the soft tissues, including tendons and bursa
- X-rays: Useful for excluding hip joint arthritis, fractures, or bone spurs that may be contributing to your symptoms
A correct diagnosis is essential to guide effective treatment. Dr Awwad’s thorough assessment aims to distinguish bursitis from other causes of lateral hip pain, such as gluteal tendinopathy or referred pain from the lower back.
Non-surgical treatment options for hip bursitis
1. Activity modification
- Avoiding activities that worsen symptoms (e.g. prolonged walking, running, or lying on the affected side)
- Short-term rest to allow inflammation to settle, especially after flare-ups
2. Anti-inflammatory medications
- Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or meloxicam may help reduce pain and swelling
- These may be used short-term and under guidance from your GP or specialist
3. Physiotherapy
- Stretching of the iliotibial band (ITB), gluteal muscles, and hip flexors
- Strengthening exercises for the gluteal muscles and core to improve hip stability
- Postural correction and gait retraining to reduce stress on the lateral hip
- Manual therapy and soft tissue massage to relieve tension and support mobility
Dr George Awwad often works collaboratively with physiotherapists to ensure your program is tailored to your symptoms and functional goals.
4. Corticosteroid injection
- If pain persists despite rest and physiotherapy, a corticosteroid injection into the trochanteric bursa may be recommended
- This can provide targeted relief from inflammation and reduce pain in the short to medium term
- Injections are typically performed under ultrasound guidance to ensure accurate placement
5. Ice and supportive therapies
- Applying ice packs to the affected area (15–20 minutes, a few times a day) can help control inflammation
- Use of a cushioned seat, pillow, or padded support while sleeping on your side may improve comfort
When might surgery be considered?
Persistent pain despite conservative treatment
Associated conditionsnservative treatment
- Gluteus medius or minimus tendon tears (often referred to as “rotator cuff tears of the hip”)
- External snapping hip syndrome
- Structural abnormalities that create ongoing irritation of the bursa
Types of surgery that may be offered
- Endoscopic bursectomy: A minimally invasive procedure to remove the inflamed bursa using small instruments and a camera
- Gluteal tendon repair: If imaging shows significant tendon tears, these may be repaired at the same time as bursa removal
- ITB release: In patients with tight iliotibial bands contributing to the condition, a lengthening procedure may be considered
Tips for prevention and long-term management
1. Maintain hip strength and flexibility
Engaging in regular strengthening and stretching exercises for the gluteal, core, and thigh muscles can help stabilise the hip joint and reduce excess strain on the bursa. A physiotherapist can tailor a program to suit your specific biomechanics and lifestyle.
2. Avoid repetitive overuse
- Long-distance running without adequate rest
- Frequent stair climbing
- Prolonged side-lying on hard surfaces
3. Use proper footwear and orthotics if needed
Wearing well-cushioned, supportive shoes and addressing any leg-length discrepancies with orthotics may help reduce hip strain caused by poor biomechanics or uneven weight distribution.
4. Optimise your body weight
Carrying excess body weight can increase mechanical stress on your hips. If appropriate, working towards a healthy weight through balanced nutrition and regular low-impact activity may reduce irritation around the bursa.
5. Treat associated conditions early
- Gluteal tendinopathy
- Hip osteoarthritis
- IT band tightness or snapping hip syndrome
6. Listen to your body
Persistent hip pain should not be ignored. Seeking early assessment and care may help prevent chronic inflammation and the development of compensatory issues in the back, knees, or opposite hip.
Frequently asked questions about hip bursitis
Is hip bursitis the same as arthritis?
Can hip bursitis go away on its own?
Is walking good or bad for hip bursitis?
Can physiotherapy help?
What happens if hip bursitis is left untreated?
Is surgery common for hip bursitis?
Surgery is usually only considered when non-surgical treatments have failed and the bursitis is significantly affecting your daily life. Dr Awwad can advise you if surgical removal of the bursa (bursectomy) or other procedures may be suitable in your case.
