Avascular Necrosis of the Hip

A loss of blood supply to the hip bone leading to joint collapse and chronic pain
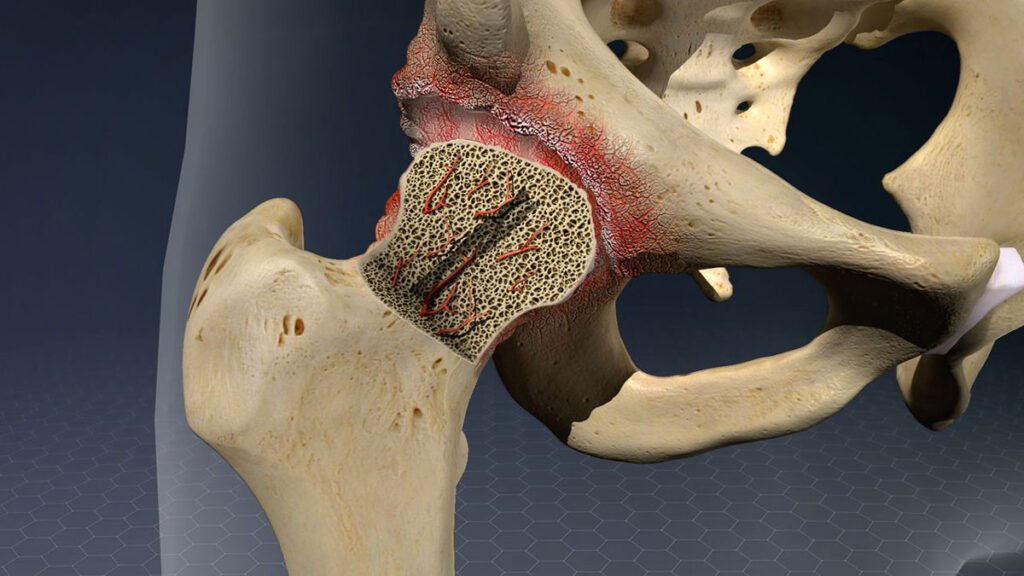
Avascular necrosis (AVN) of the hip, also referred to as osteonecrosis, is a condition where the blood flow to the femoral head (the ball portion of your hip joint) becomes reduced or completely interrupted. Without adequate circulation, the bone tissue begins to die, leading to weakening and eventual collapse of the joint surface. Over time, this can result in severe pain, stiffness, and the development of hip arthritis.
AVN often affects adults between the ages of 30 and 60 and can sometimes progress silently in the early stages. As the condition worsens, the structural integrity of the femoral head deteriorates, increasing the risk of joint dysfunction, instability, and reduced mobility.
Dr George Awwad offers a comprehensive assessment and management plan for patients with AVN of the hip. Depending on the stage of the disease, treatment may aim to preserve the native joint or, in more advanced cases, relieve symptoms and restore function through hip replacement surgery.
What causes avascular necrosis of the hip?
Avascular necrosis (AVN) of the hip develops when the blood supply to the femoral head becomes disrupted or significantly reduced. Without adequate blood flow, the bone cells in the hip begin to die, which can weaken the bone structure, lead to joint collapse, and eventually cause arthritis.
Traumatic causes
-
Hip fracture or dislocation
Injury to the hip joint, particularly femoral neck fractures or dislocations, can damage the blood vessels that supply the femoral head. This is a common cause of AVN, particularly in younger or middle-aged adults after trauma.
Non-traumatic causes
-
Corticosteroid use
Long-term or high-dose corticosteroid therapy is one of the most common non-traumatic causes of AVN. The exact mechanism is not fully understood but may involve increased fat in the blood that narrows small blood vessels. -
Excessive alcohol intake
Chronic alcohol consumption may interfere with bone metabolism and impair circulation to the femoral head. -
Medical conditions
AVN is associated with several systemic conditions, including:
- Sickle cell disease
- Lupus (systemic lupus erythematosus)
- Blood clotting disorders (thrombophilia)
- Gaucher’s disease
- Decompression sickness (in divers or pilots)
-
Certain treatments
AVN may occasionally develop following radiation therapy, chemotherapy, or organ transplantation.
Idiopathic cases
In some individuals, no clear cause can be identified. These cases are referred to as idiopathic AVN. Even without a known cause, the disease process and progression remain similar.
Symptoms of avascular necrosis
Early symptoms
- Intermittent hip pain – initially mild, often brought on by weight-bearing activities such as walking or climbing stairs.
- Groin discomfort – pain is often felt deep in the groin, but it may also radiate to the thigh or buttock.
- Stiffness – a feeling of tightness in the hip joint, particularly in the morning or after periods of inactivity.
Progressive symptoms
- Persistent pain – discomfort becomes more constant, occurring even at rest or during the night.
- Limping – altered walking pattern due to pain, stiffness, or instability in the hip.
- Clicking or catching sensations – some patients notice mechanical symptoms as the bone surface loses its smooth contour.
Advanced stage symptoms
- Severe pain – often limiting daily activities and significantly impacting quality of life.
- Joint deformity – progressive changes in hip alignment as the joint surface deteriorates.
- Secondary arthritis – as the bone collapses, the cartilage is damaged, leading to painful arthritis and further loss of function.
How is avascular necrosis diagnosed?
Clinical assessment
- Review of your medical history – including any history of steroid use, alcohol intake, previous trauma, or underlying health conditions that may increase your risk.
- Discussion of symptoms – including the location, intensity, and timing of your hip pain or stiffness.
- Physical examination – to assess your range of motion, muscle strength, joint tenderness, and gait pattern.
Imaging studies
- X-rays – often the first imaging test performed. In early AVN, X-rays may appear normal, but in later stages, they can reveal changes such as bone collapse or joint space narrowing.
- MRI (Magnetic Resonance Imaging) – the most sensitive imaging method for early AVN. MRI can detect subtle changes in bone tissue before they are visible on an X-ray, helping identify the condition in its earliest, most treatable stages.
- CT scans (Computed Tomography) – may be used to assess the extent of bone collapse or to assist with surgical planning in more advanced cases.
- Bone scans – sometimes used when MRI is not available or contraindicated. These can show areas of reduced or absent blood flow in the femoral head.
Staging the disease
Stages of avascular necrosis
Stage 0: pre-clinical
- Description: No symptoms are present and imaging tests (like X-rays) appear normal.
- Detection: AVN may only be detected by an MRI, which can reveal early bone changes not yet visible on X-ray.
- Treatment goal: Early detection may allow for joint-preserving measures such as activity modification, medication, or offloading the joint.
Stage 1: early stage
- Description: Symptoms such as mild hip pain may begin to develop, but X-rays remain normal.
- MRI findings: Changes in bone marrow or subtle damage to the blood supply become visible.
- Treatment goal: Focus is on preserving the joint and slowing disease progression through non-surgical options.
Stage 2: structural changes without collapse
- Description: X-rays now show signs of AVN such as sclerosis (increased bone density) or cystic changes, but the shape of the femoral head is still maintained.
- Symptoms: Hip pain becomes more noticeable, especially with weight-bearing activities.
- Treatment goal: Continue joint-preserving strategies, though surgical intervention may be considered for selected patients.
Stage 3: femoral head collapse
- Description: The femoral head begins to flatten or collapse, indicating significant bone death.
- Imaging findings: Crescent sign on X-ray, indicating a fracture under the surface of the bone.
- Symptoms: Pain increases, and mobility may be reduced.
- Treatment goal: Joint-preserving surgery may no longer be effective; joint replacement is often recommended at this stage.
Stage 4: joint space narrowing and arthritis
- Description: Advanced joint destruction occurs, with narrowing of the joint space, cartilage loss, and secondary osteoarthritis.
- Symptoms: Persistent pain, stiffness, and difficulty with walking or daily activities.
- Treatment goal: Total hip replacement surgery is typically required to restore joint function and relieve pain.
Non-surgical treatment options for avascular necrosis
Activity modification and offloading
- Use of crutches or walking aids to assist with mobility and reduce joint load.
- Avoiding high-impact activities such as running or jumping.
- Modified work duties or lifestyle adjustments may be recommended depending on the severity of symptoms.
Pain management
- Anti-inflammatory medications (NSAIDs) such as ibuprofen or meloxicam may help reduce pain and swelling.
- Simple analgesics such as paracetamol can be used for regular pain control.
Physiotherapy and exercise
- Gentle stretching and strengthening exercises to support the surrounding muscles.
- Aquatic therapy or low-impact activities such as swimming or cycling may be advised.
Medications to support bone health
- Bisphosphonates (e.g. alendronate) may reduce bone loss.
- Lipid-lowering agents (e.g. statins) may be helpful in patients with underlying lipid disorders.
- Anticoagulants may be used in rare cases where AVN is linked to blood clotting disorders.
Biological and injection therapies (emerging options)
- Core decompression combined with biologics may be offered as part of a joint-preserving surgical strategy in early-stage AVN.
- Stem cell or bone marrow concentrate injections aim to stimulate bone regeneration.
Close monitoring
In all non-surgical cases, regular monitoring with imaging (such as MRI or X-ray) is essential to assess disease progression and determine whether surgical intervention becomes necessary.
Surgical treatment for AVN of the hip
Core decompression (with or without biologics)
- May be performed in the early stages (pre-collapse) of AVN.
- Often combined with bone grafting or biologic treatments such as bone marrow aspirate concentrate (BMAC) or stem cells.
- Suitable for younger patients or those with small, localised lesions.
Bone grafting procedures
- Vascularised bone grafts (such as from the fibula) bring a live blood supply to the area.
- Non-vascularised grafts may also be used in less complex cases.
- These procedures are technically demanding and are typically considered in selected patients under specialist orthopaedic care.
Osteotomy
- Most commonly used in younger patients with early or mid-stage AVN.
- Aims to preserve the hip joint and delay the need for total hip replacement.
- Requires a longer recovery period and has variable long-term results.
- Involves replacing the damaged ball-and-socket joint with a prosthetic implant.
- Offers reliable pain relief, improved function, and restoration of mobility.
- Dr George Awwad uses anterior approach techniques, which may support faster recovery and reduce post-operative discomfort.
- THR may be the preferred option for patients with advanced-stage AVN or those who are no longer suitable for joint-preserving procedures.
Choosing the right surgical approach
- Stage of AVN (assessed using imaging)
- Age and activity level of the patient
- Size and location of the necrotic area
- Presence of underlying conditions (e.g. steroid use, alcohol intake, trauma)
- Patient’s goals and overall hip function
Long term outcomes and follow-up care with AVN
Prognosis depends on the stage and treatment
- The stage of the disease at the time of diagnosis
- The size and location of the necrotic area
- The underlying cause (e.g. trauma, steroid use, alcohol intake, systemic conditions)
- Whether the femoral head has collapsed
- The timing and type of treatment (non-surgical or surgical)
Potential long-term complications
- Progressive femoral head collapse
- Hip joint arthritis
- Loss of mobility
- Chronic pain
- Reduced quality of life
Regular monitoring and imaging
- Repeat X-rays or MRIs may be recommended every 3–6 months to assess progression.
- Your imaging results guide decisions on whether further treatment (such as surgery) may be required.
Lifestyle modifications and risk reduction
- Avoiding corticosteroids unless medically necessary
- Minimising alcohol consumption
- Weight management to reduce joint load
- Limiting high-impact activities if the femoral head is vulnerable
- Managing underlying conditions (e.g. lupus, blood disorders)
Long-term care after surgery
- Monitor implant integrity
- Check for signs of wear, loosening, or infection
- Assess your functional progress
- Support your rehabilitation and return to activity
