Hip Arthritis
A degenerative joint condition that may cause pain, stiffness, and reduced mobility
Hip arthritis is a progressive condition that affects the smooth cartilage lining of the hip joint, leading to inflammation, joint damage, and discomfort during movement. As the cartilage wears away over time, the bones may begin to rub together, causing pain, stiffness, and reduced range of motion. This condition can have a significant impact on your ability to walk, exercise, work, or enjoy everyday activities. While hip arthritis is often associated with ageing, it can also affect younger people due to injury, joint abnormalities, or underlying health conditions.
Dr George Awwad provides comprehensive assessment and care for patients living with hip arthritis, offering a wide range of non-surgical and surgical treatment options tailored to your lifestyle and needs. This page explains what hip arthritis is, common symptoms to look out for, and how it may be managed.
What causes hip arthritis?
Hip arthritis occurs when the cartilage that lines the hip joint gradually wears away or becomes damaged. This protective cartilage allows the ball-and-socket joint of the hip to move smoothly. When it breaks down, the bones can rub together, leading to pain, stiffness, and inflammation. Several factors may contribute to the development of hip arthritis:
Age-related joint wear (Osteoarthritis)
Osteoarthritis is the most common cause of hip arthritis and is often associated with ageing. Over time, the cartilage in the hip joint may naturally degenerate due to years of repetitive use, leading to joint changes that cause discomfort and reduced mobility.
Previous hip injury or trauma

Structural abnormalities (Hip dysplasia or impingement)
Some people are born with differences in the shape of their hip joint. Conditions like hip dysplasia or femoroacetabular impingement (FAI) can cause uneven loading or restricted motion in the joint, accelerating cartilage wear and increasing the risk of early arthritis.
Inflammatory conditions
Genetic factors
Obesity and joint load
Lifestyle and activity level
Types of hip arthritis
Osteoarthritis (OA)
Rheumatoid arthritis (RA)
Post-traumatic arthritis
Psoriatic arthritis
Ankylosing spondylitis
Avascular necrosis (osteonecrosis)
Common symptoms of hip arthritis
Hip pain
Stiffness
Reduced range of motion
Limping or altered walking pattern
Activity-related discomfort
Clicking or grinding sensation
Diagnosing the type of arthritis affecting your hip
Clinical consultation and history
Physical examination
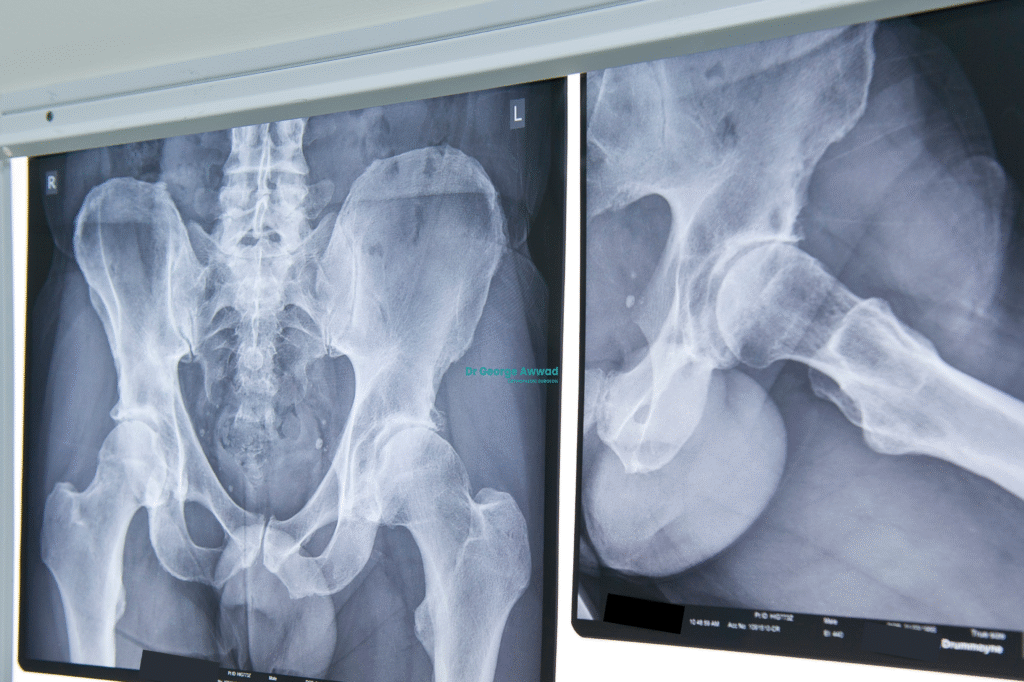
X-rays
Advanced imaging
Blood tests
Non-surgical hip arthritis treatment options
Lifestyle and activity modifications
- Avoiding repetitive twisting or high-impact movements
- Using mobility aids such as a walking stick for support
- Modifying work duties or sports that aggravate symptoms
Physiotherapy
Medications
- Paracetamol: Often used as a first-line option for mild pain.
- Non-steroidal anti-inflammatory drugs (NSAIDs): Such as ibuprofen or meloxicam, which can help reduce inflammation and provide relief.
- Topical anti-inflammatory gels: These may offer localised relief with fewer systemic side effects.
- Prescription medications: In cases of inflammatory arthritis, disease-modifying antirheumatic drugs (DMARDs) or biologic therapies may be recommended by a rheumatologist.
Injections
- Corticosteroid injections: Can reduce inflammation and pain within the joint.
- Hyaluronic acid injections: Sometimes used to supplement joint lubrication, although evidence in the hip is less established. Injections are not a long-term cure, but they may delay the need for surgery in certain cases.
Walking aids and orthotic support
When surgery may be considered
If non-surgical treatments no longer provide adequate relief, or if hip arthritis begins to significantly affect your ability to perform daily activities, hip replacement surgery may be considered. Dr Awwad will assess your symptoms, imaging results, and overall health to determine whether surgery is an appropriate next step.
Signs that surgery may be appropriate
- Persistent or worsening hip pain despite medications and physiotherapy
- Difficulty walking, climbing stairs, or getting out of chairs
- Reduced range of motion that limits independence or quality of life
- Sleep disturbance due to hip pain
- Reliance on walking aids without significant improvement
Individualised decision-making
The decision to proceed with surgery is always individual. Dr Awwad will consider:
- The severity of joint damage seen on X-rays or other imaging
- The impact of symptoms on your lifestyle, work, and mobility
- Your overall health and any medical conditions that could influence recovery
- Your personal goals and expectations from surgery
